Dosing Strategy and Final Pearls for Nirsevimab for RSV
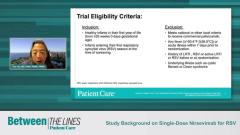
Experts conclude their discussion on the efficacy and safety study of nirsevimab for Respiratory Syncytial Virus (RSV) commenting on possible dosing strategies and key takeaways from this study.
Episodes in this series

Transcript
Tina Tan, MD, FAAP, FIDSA, FPIDS: Now that the nirsevimab has been approved, one question people have is: Should this be administered prior to discharge from the nursery, or should they need to come back during the first couple weeks of life in order to get the monoclonal? What’s your opinion of this?
Flor M. Munoz, MD, MSc: I think that having the ability to provide protection at a high efficacy—75%—is pretty good against medically important, medically attended lower respiratory tract illness or bronchiolitis in these babies. So the earlier, the better in terms of the respiratory season and in terms of the age of the baby. Because again, we might not have seen that much of an impact here with the [babies who were] less than 5 kg—which would be our newborns—but it might also be an issue of the number of cases that occurred. So if we have an option to…know when RSV [respiratory syncytial virus] is circulating in the community, then to give this monoclonal antibody as soon as the baby is ready to go home, when you know RSV season is about to start or already started, definitely when it’s already RSV season, more important even to give it as soon as the baby is leaving the hospital. If the baby is born in August or July, you do have the option because the period of administration went up to several months after birth, so you would have the option to wait a little [longer] and give it as an injection when you know RSV is about to start. The tricky part is knowing when RSV is starting and being very aware of your local data or [Centers for Disease Control and Prevention] data. I’m in Texas, and we know that in the southern part of the United States…we do have an early start compared [with] northern states. We also have a longer duration…of RSV season, so we would be already worried about RSV between October, [and] certainly end of September…. So I would say any baby [who] is born from October on, I would rather give it as soon as they leave the hospital for birth and not wait until after that.
Tina Tan, MD, FAAP, FIDSA, FPIDS: That’s really important and is something I hope the community pediatricians or [those who] take care of children in the community think about, because…if you’re not in the middle or getting set to start RSV season when the baby’s born, it’s going to be better if they wait a couple months to get the monoclonal so they have protection through the RSV season. That’s going to be really important for community practitioners to think about so they can stock it in their offices.
Flor M. Munoz, MD, MSc: It’s very similar to…how the decisions were made around palivizumab for the very preterm babies. We were always watching for the RSV season and we had definitions [for] when [it was] considered to be a season and when the virus [was] circulating so we could start. The difference was, as you mentioned, that you needed monthly administrations, and even then [there was] a little bit harder [of a] start of the effect because maybe 1 dose was not sufficient to really prevent all the infections. But when you had 2 or 3 doses in those babies, you had a better effect and protection. In this case, it really is a matter of getting that first dose in and [being] able to have the protection for a longer period of time. There’s always a balance, but it’s the same concept. I think pediatricians are used to that. What we’re not used to maybe is actually being the ones who administer this.
Tina Tan, MD, FAAP, FIDSA, FPIDS: Exactly, and especially to older preterm infants, or older late preterm infants and normal healthy term infants. So that’s going to be something that’s a little different.
Flor M. Munoz, MD, MSc: A little different. And again, the communication is going to be important between the hospital where the babies are born and the pediatricians. Fortunately, most babies already have a pediatrician when they’re born—I hope so. So they will be aware, and they might be the ones actually ordering it. It’s just going to be given at the hospital. But we also have opportunities; a lot of pediatricians like to see their babies in their first 2 weeks of life to make sure they’re gaining weight and all of that. That is another opportunity right there, as well, to do it in their office.
Tina Tan, MD, FAAP, FIDSA, FPIDS: Flor, I want to thank you so much for this really informative discussion. I hope you and the viewers enjoyed this Between the Lines Journal Club experience. Thank you for tuning in.
Flor M. Munoz, MD, MSc: Thank you so much, Tina.
Transcript is AI-generated and edited for clairty.
Newsletter
Enhance your clinical practice with the Patient Care newsletter, offering the latest evidence-based guidelines, diagnostic insights, and treatment strategies for primary care physicians.