
32-year-old man presents with a 4-day history of fever (temperature as high as 38.8 C to 39.4 C with severe rigors, chills, and profuse night sweats; generalized myalgias, including dull, aching headache; and dry cough.

32-year-old man presents with a 4-day history of fever (temperature as high as 38.8 C to 39.4 C with severe rigors, chills, and profuse night sweats; generalized myalgias, including dull, aching headache; and dry cough.

Stories about community-associated infections with methicillin-resistant Staphylococcus aureus (MRSA) have been making headlines in recent months in both the medical and popular press. A familiar problem in hospitals and nursing homes for decades, growing numbers of MRSA infections have been documented over the past few years in prison inmates, soldiers, athletes, Pacific Islanders, Alaska Natives, Native Americans, and men who have sex with men.

A 42-year-old woman presents with severe diarrhea that began 3 days earlier and has become progressively more severe. She is now having 10 or more watery bowel movements per day. She has had moderate nausea but no emesis, hematemesis, or hematochezia.

Anorectal abscesses and fistulae, pilonidal disease, rectal prolapse, pruritus ani, and anal masses are discussed, with an emphasis on diagnosis and treatment of these conditions in the primary care office setting.

Anorectal complaints are commonly seen in primary care practice. The two most common anorectal conditions are hemorrhoids and anal fissures.

This case highlights the importance of detecting HIV infection in its earliest stages. Each year, 40,000 new cases of HIV infection are diagnosed in the United States; however, very few of these are identified at the acute infection stage. Diagnosis of primary HIV infection is important because it improves the patient's chances for a good outcome, reduces the risk of transmission, and provides epidemiologic data on virus strains in the community.

A 13-year-old boy presented with an explosive eruption of numerous, small, round, erythematous, itchy plaques on his lower back and lower limbs of 2 weeks' duration. Some of the lesions were scaly. His nails were normal. There was no evidence of arthritis or joint deformity. He had a sore throat a month before the onset of the rash but did not seek medical attention. He was not taking any medication and had no history of joint pain or family history of skin problems.

An 80-year-old man complains of lancinating pain in his right axilla and chest that began 2 days earlier and has kept him awake at night. He has had no fever, cough, sputum production, dyspnea, or symptoms suggestive of congestive heart failure.

Abstract: The use of sputum studies and blood cultures in patients hospitalized with community-acquired pneumonia (CAP) is somewhat controversial, and recommendations continue to evolve. A reasonable approach is to attempt to obtain sputum cultures from all patients before initiating antibiotic therapy. If antibiotics have already been given, sputum studies can be reserved for patients who are severely ill or who are at risk for infection with a resistant organism or an organism that is not covered by the usual empiric therapy. The Infectious Diseases Society of America and the American Thoracic Society both recommend obtaining blood cultures from all patients. However, cost considerations have led to alternative strategies, such as reserving blood cultures for those with severe CAP. (J Respir Dis. 2005;26(4):143-148)

A 38-year-old man presented to the emergency department (ED) with a 2-week history of worsening shortness of breath and dry cough. He also complained of anorexia, a 14-kg (30-lb) weight loss over 3 months, pleuritic chest pain, and night sweats.

A 45-year-old Asian man presents with a 3-week history of weight loss, poor appetite, fatigue, intermittent sweats, and a nonproductive cough. The patient, a recent immigrant, denies previous illness.

ABSTRACT: Although the widespread use of prostate-specific antigen (PSA) testing has led to an increase in the number of cancers detected, controversies about the benefits of screening persist. No conclusive evidence has yet emerged that PSA screening reduces the mortality associated with prostate cancer. Thus, mass screening is not universally endorsed. The American Urologic Association and the American Cancer Society recommend that digital rectal examination and PSA testing be offered annually to men 50 years and older with an estimated life expec- tancy of 10 years or more. High-risk patients (those with a positive family history or those of African American descent) are advised to begin screening at age 45. The decision to screen is based on the patient's preference following a thorough discussion of the benefits and limitations of PSA testing. Refer to a urologist any patient with a PSA greater than 4.0 ng/mL. Also, be alert for high PSA velocity changes in patients undergoing annual screening, and refer those with a PSA velocity of more than 0.75 ng/mL/y.

ABSTRACT: Rely on the history and physical findings when you evaluate a hand injury. After you control any active bleeding, test the motor and sensory functions of the radial, ulnar, and medial nerves. Use the rule of the 5 P's-pulses, pallor, pain, paresthesia, and paralysis-to guide the vascular examination. Assess the muscles and tendons by testing their flexion and extension functions against mild resistance. After anesthetizing any wound sites, apply high-pressure saline irrigation to remove debris and reduce bacterial contamination to prevent infection. To repair skin injuries, use a closure method appropriate to the condition of the wound. Infection-prone wounds-such as crush, grossly contaminated, and bite injuries-may require antibiotic prophylaxis and possibly delayed closure.

ABSTRACT: The rate at which acute dyspnea develops can point to its cause. A sudden onset strongly suggests pneumothorax (especially in a young, otherwise healthy patient) or pulmonary embolism (particularly in an immobilized patient). More gradual development of breathlessness indicates pulmonary infection, asthma, pulmonary edema, or neurologic or muscular disease. A chest film best identifies the cause of acute dyspnea; it can reveal pneumothorax, infiltrates, and edema. Pulmonary embolism is suggested by a sudden exacerbation of dyspnea, increased ventilation, and a drop in PaCO2. A normal chest radiograph reinforces the diagnosis of pulmonary embolism, which can frequently be confirmed by a spiral CT scan of the chest. Pneumonia can be difficult to distinguish from pulmonary edema. In this setting, bronchoalveolar lavage and identification of the infectious organism may be necessary to differentiate between the 2 disorders.

ABSTRACT: Asymmetry-whether of strength, reflexes, or sensory function-is an important localizing finding in the neurologic evaluation. Asymmetric deficits of strength may indicate an acute CNS lesion. Symmetric hyperreflexia or hyporeflexia alone is not diagnostic; compare reflexes between sides of the body and between upper and lower extremities. The extensor plantar response (Babinski reflex) suggests an upper motor neuron lesion. During the sensory examination, look for asymmetry and determine whether both light touch and pinprick sensation are intact. Simultaneous stimulation with 2 sharp objects on opposite sides of the body-done to detect extinction of response on 1 side-can uncover subtle sensory deficits.

ABSTRACT: When you approach a patient with a neurologic complaint, look for abnormal postures and bodily asymmetries. Careful history taking puts the patient's complaint in context and gives direction to the clinical investigation. Remember that a change in the character of an existing condition requires assessment as a new complaint. The mental status evaluation, at a minimum, considers the patient's level of alertness and orientation, including speech and comprehension. Distinguish among delirium, dementia, and psychosis, and avoid making a psychiatric diagnosis until organic causes have been excluded. Cranial nerves II to VIII are the most pertinent to the neurologic screening examination. The evaluation of cranial nerves II, III, IV, and VI is particularly important in patients with headache or visual disturbances and suspected intracranial lesions.

A 30-year-old man has had painful genital lesions for the pastseveral days. He recently returned from a business trip during which hehad several unprotected sexual encounters.
A 48-year-old man with jaundice, nausea, vomiting, and abdominal pain was hospitalized. The patient- a recovering alcoholic- was afebrile and reported abstinence from alcohol for 6 months.

ABSTRACT: The complexities of chronic nonmalignant pain and the contributions of psychosocial and environmental factors require assessment and treatment strategies that may go far beyond the use of analgesics. The first step is to rule out serious underlying conditions; determine the chronicity, quality, location, and intensity of the pain; assess aggravating environmental factors; and evaluate the patient's level of functioning. The pharmacologic regimen may include oral or topical analgesics, antidepressants, muscle relaxants, nerve stabilizers, and/or opioids. A comprehensive plan includes alternative modalities, such as physical and occupational therapy, stress management, relaxation techniques, and the treatment of comorbid conditions, including anxiety, depression, and sleep disorders. The optimal opioid regimen consists of methadone or a sustained-release opioid combined with a short-acting opioid for breakthrough pain.

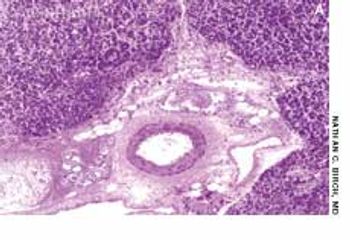
35-year-old Hispanic man presented with nonproductive cough; dyspnea; fever; and a painful, ulcerated, 1.5-cm, red-brown plaque on the left flank. He had had the lesion for 3 months and the symptoms for 1 week. The patient had grown up in Arizona, and he traveled there 4 months before the lesion arose.

Routine inspection of the oral cavity is not a part of every patient encounter. There exist, nevertheless, clear indications for physical examination of the mucosal surfaces between the lips and the anterior tonsillar pillars; these include symptoms such as pain, erythema, and swelling that are referable to this area.

ABSTRACT: Acute and recurrent cystitis in young women, once identified, can be treated empirically without microbiologic confirmation. In these women, a urine dipstick test that is positive for nitrates or leukocyte esterase is considered diagnostic. The usual treatment is a 3-day course of an antibiotic. Prophylaxis is recommended for women who have more than 3 episodes of cystitis per year. Options include postcoital prophylaxis with a single dose of antibiotic or long-term low-dose antimicrobial therapy. In young women with acute pyelonephritis, fluoroquinolones are the treatment of choice. Empiric therapy is initiated as soon as possible in patients at risk for complicated urinary tract infections (UTIs). Alternative techniques, such as intermittent catheterization, may reduce the incidence of UTIs in patients with indwelling catheters.

Recreational diving continues to increase in popularity; as many as 15 million Americans are certified scuba divers. Although a few serious and possibly life-threatening conditions require recompression treatment, most diving injuries are uncomplicated and can be managed by the primary care physician. In this article, we address the questions most often asked about fitness and safety issues. In a future article, we will review the principal medical problems associated with sport diving.

A 40-year-old womanwith HIV infection has had an occasionallypruritic facial rash for severalmonths. The rash is not associatedwith any systemic symptoms.

During the past week, a rash on theright thumb and forefinger of a 4-yearoldboy has progressed to involve theentire arm.