COPD Exacerbations May Increase Risk of Severe CV Events by More Than 15-Fold: Cohort Study
The risk of severe CV events, including leading to death, was greatest in the first week following an exacerbation but remained significantly elevated 1 year later.
Exacerbations of chronic obstructive pulmonary disease (COPD) increased the risk of severe cardiovascular (CV) events by nearly 16-fold in the week following the exacerbation with the greatest risk observed for heart failure (HF) decompensation and arrhythmias, according to findings from a new study by Canadian investigators.
While risk was highest during days 1-7 post exacerbation, it remained elevated for up to 1 year for all CV outcomes evaluated and beyond 1 year for acute coronary syndrome (ACS) and all-cause mortality, the Canadian team reported in the journal Heart. The ongoing risk was associated with moderate as well as severe exacerbations.
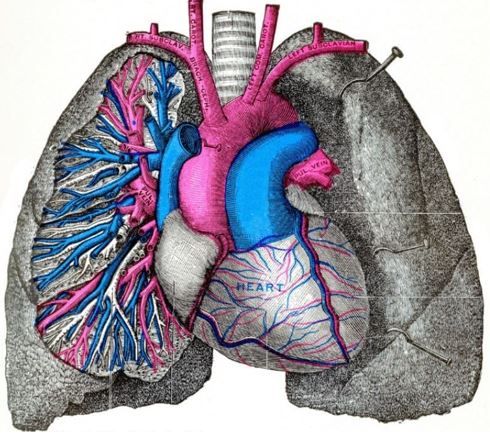
©Morphart Creations/shutterstock.com
Over the study's 5-year follow-up period, nearly half (43.4%) of the 142 787 participants had at least 1 COPD exacerbation of any severity, according to the findings. Of the 23.9% of participants who died, approximately one-third (29.7%) died of cardiac-related outcomes.
"Patients who experience [COPD] exacerbations are treated across diverse medical specialties including primary care, respirology, cardiology and internal medicine," Nathaniel Hawkins, MBChB, MD, MPH, assistant professor, University of British Columbia, and colleagues wrote. They concluded that "exacerbations of COPD are independent and modifiable risk factors for severe CV events," and urged all health care professionals who care for people with COPD to "optimize strategies to prevent exacerbations and mitigate this heighted CV risk." Preventive strategies they recommend include minimizing exposure to potential triggers, self-management, inhaled maintenance therapies, and other CV risk factor screening and treatment.
CV disease and risk factors are common in patients with COPD, with HF and arrhythmias observed in 42% and 21% of those living with the disease, respectively, Hawkins et al wrote. The investigators cite evidence in particular for increased risk of myocardial infarction (MI), stroke, and CV mortality during and directly following an exacerbation, but also note that previous research has focused on these outcomes with only scant attention paid to others, notably HF and arrhythmias, within composite endpoints, Also limiting applicability of previous studies to real world experience are conflicting findings regarding the risk of CV events as related to exacerbation history and follow up times described as variable and frequently truncated. "Altogether, the relationship between exacerbation severity and a broader range of CV outcomes is unknown in a general population with extended follow-up."
For their retrospective cohort study the team identified individuals with COPD using administrative data from Alberta Health's multidatabase COPD chronic disease cohort, selecting participants between April 1, 2014, and March 31, 2019, with cutoff dates identifying those considered to have prevalent disease and those considered newly diagnosed. Study inclusion required age of 40 years or older, data available for at least 24 months before study entry and no diagnosis of COPD related to alpha-1 antitrypsin deficiency. Follow-up ended at first occurrence of an outcome of interest or censoring.
Outcomes of primary interest to Hawkins and colleagues were hospitalization of at least one night for ACS, HF decompensation, a new diagnosis of arrhythmia, or cerebral ischemia and all-cause death. Endpoints considered were time to a first non-fatal CV event or death (composite outcome) and (2) time to each individual non-fatal CV event or death. Covariate-adjusted risks associated with 6 exposure subperiods following exacerbation were estimated.
FINDINGS
The final cohort of 142 787 participants had an average age of 68.1 years and half (51.7%) were men. Just more than one-third (37.1%) were identified as newly diagnosed with COPD. The majority (81.8%) had not experienced a COPD exacerbation in the year before study entry, 14.5% had had 1 exacerbation, and 3.6% had had 2 or more. Cardiovascular risk factors and comorbidities reported by more than 10% of participants are listed in the Table.
Researchers recorded the primary composite outcome in 30.5% of study participants. The pre-exacerbation rate of 5.43 (95% CI, 5.36 - 5.50) per 100 person-years (PY) increased nearly 16-fold to 95.61/100 PY in the 1–7 days post-exacerbation (adjusted HR 15.86; 95% CI, 15.17-16.58). Although the risk declined with time, Hawkins et al reported a significant incidence rate of 7.3 at 1 year after an exacerbation (95% CI, 7.16-7.55; HR 1.08, 95% CI, 1.05-1.12).
When investigators looked specifically at individual CV outcomes they found a significant risk for all of them after any level of COPD exacerbation that was higher in the earlier periods. They highlighted the notably increased comparable risk for HF decompensation, which rose from a rate of 0.56/100 PY before a first exacerbation event to a rate of 21.45/100 PY in the first 7 days. They emphasized that between 31 and 180 days, the incidence rate for HF decompensation remained significantly elevated (0.68; 95% CI 0.61-0.76; aHR 2.25; 95% CI, 1.96-2.59).
"Our real-world findings of elevated risk for a broad range of cardiac events and all-cause death, persisting for 1 year or more, including first and subsequent exacerbations, emphasise the burden of cardiopulmonary risk in patients living with COPD," wrote Hawkins and colleagues in their discussion. "Once exacerbations occur, therapies and risk stratification for both cardiac and pulmonary disease should be revisited and intensified. Multidisciplinary team-based approaches are needed to address the complex interaction between lung and cardiac dysfunction," they concluded.
Source: Hawkins NM, Nordon C, Rhodes K, et al. Heightened long-term cardiovascular risk after exacerbation of chronic obstructive pulmonary disease. . 2024;0:1–8. doi:10.1136/heartjnl-2023-323487
Newsletter
Enhance your clinical practice with the Patient Care newsletter, offering the latest evidence-based guidelines, diagnostic insights, and treatment strategies for primary care physicians.