CV Risk Factors Increasing Among Middle-Aged US Adults, Socioeconomic Inequities Persist: New Findings
A study of more than 20 000 middle aged US adults over the past 2 decades found that lower income status was consistently associated with higher rates of hypertension, diabetes, and cigarette use while diabetes and obesity increased among higher income adults in the same age cohort.1
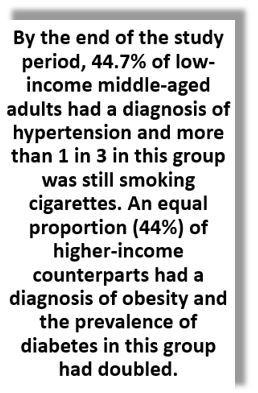
The study, led by investigators at Beth Israel Deaconess Medical Center (BIDMC) in Boston, MA, using data on adults aged 40 to 60 years from the National Health and Nutrition Examination Survey (NAHNES) for the years 1999 to March 2020, revealed among other findings, an increase in hypertension among low-income adults from 37.2% to 44%.7% over the study period while the prevalence of diabetes and obesity was unchanged.1
©Sebastien Garcia/stock.adobe.com
In contrast, while hypertension prevalence did not change among higher income adults, diabetes nearly doubled (7.8% to 14.9%) and obesity rose from 33.0% to 44.0%.1 Of significant concern, according to the study findings, by the end of the study period, nearly 1 in 2 middle-aged adults had obesity regardless of income level.1
According to data from the Centers for Disease Control and Prevention declines in US cardiovascular (CV) mortality observed during the latter half of the 20th century have stalled,2 a trend driven in part by an increase in deaths among middle-aged adults and particularly among those of lower socioeconomic status, the authors wrote in the Annals of Internal Medicine. This is a population already disproportionately affected by social determinants linked to poor cardiovascular health, they emphasize, but research is scarce on how the burden of CV risk factors may have changed over time among middle-aged adults when parsed by income level over the past 2 decades.1
BDIMC researchers designed the current cross-sectional study to evaluate trends in the prevalence, treatment, and control of CV risk factors among low-income and higher-income middle-aged adults and how social determinants contribute to recent associations between income and CV health.
The research team identified NHANES participants aged 40 to 60 years who had completed the household interview and medical examination components of the survey from 1999 through March 2020. The unweighted final cohort numbered 20 761 participants. Mean age was 51.4 years and 51.4% were women.1
They examined baseline systolic blood pressure (SBP), diastolic blood pressure, HbA1c, total cholesterol, and body mass index (BMI) for all participants and then evaluated the age-standardized prevalence of hypertension, diabetes, hyperlipidemia, obesity, and current cigarette smoking. Rates of treatment and of control were determined for hypertension, diabetes, and hyperlipidemia. Income was measured by the income-poverty ratio and investigators used Department of Health and Human Services definitions to identify participants with low- and higher-income status.1
FINDINGS1
Risk factor prevalence
In addition to the findings cited above for hypertension, diabetes, and obesity, BDIMC investigators reported that current cigarette use was high and did not change among low-income adults between 1999 (33.2%) and 2020 (33.9%) but among higher-income participants, they observed a significant decrease, from 18.6% to 11.5%. Hyperlipidemia significantly decreased in both the low-income group (83.6% to 59.6%) and higher-income group (75.7% to 65.5%).
Income-based disparities in hypertension, diabetes, obesity, and cigarette use did not narrow over the study period, according to the findings.
Risk factor treatment and control
Age-adjusted treatment and control rates for hypertension among those being treated were reported as high (>80%) and unchanged over the study period in both income groups.
Treatment rates for diabetes were consistent over time for low-income adults but rose significantly for the higher-income cohort, from 58.4% to 77.4%. Conversely, rates of glycemic control among those receiving treatment in the low-income group significantly increased from 18.7% to 38.4%, but did not change in the higher-income group.
The investigators reported significant decreases in treatment rates for hyperlipidemia across income groups over the study period; however, hypercholesterolemia control among participants on treatment increased significantly for both low- (39.5% to 67.7%) and higher- (52.5% to 68.6%) income adults.
By the end of the study period, 44.7% of low-income middle-aged adults had a diagnosis of hypertension and more than 1 in 3 in this group was still smoking cigarettes. An equal proportion (44%) of higher-income counterparts had a diagnosis of obesity and the prevalence of diabetes in this group had doubled.
Income-based disparities in hypertension, diabetes, and cigarette use persisted in more recent years even after adjustment for insurance coverage, health care access, and food insecurity, according to the authors. These findings suggest that “targeted public health and policy initiatives to improve the prevention, diagnosis, and treatment of cardiovascular risk factors, particularly among low-income communities, are urgently needed to address the ongoing increase in cardiovascular mortality among middle-aged adults.”
References
1. Liu M, Aggarwal R, Zheng Z, et al. Cardiovascular health of middle-aged US adults by income level, 1999 to March 2020: A serial cross-sectional study. Ann Intern Med. 2023;176:1595-1605. doi:10.7326/M23-2109
2. Centers for Disease Control and Prevention (CDC). Decline in deaths from heart disease and stroke – United States, 1900-1999. MMWR Morb Mortal Wkly Rep. 1999;48:649-656. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm4830a1.htm
Newsletter
Enhance your clinical practice with the Patient Care newsletter, offering the latest evidence-based guidelines, diagnostic insights, and treatment strategies for primary care physicians.