New Phase 3 Data Suggest Benefits of Early Lecanemab Initiation on Alzheimer Disease Progression, Support Long-Term Safety
New data from phase 3 Clarity AD OLE trial show sustained treatment benefit among participants with low baseline tau and brain amyloid with no new safety signals.
©Lightspring/Shutterstock.com
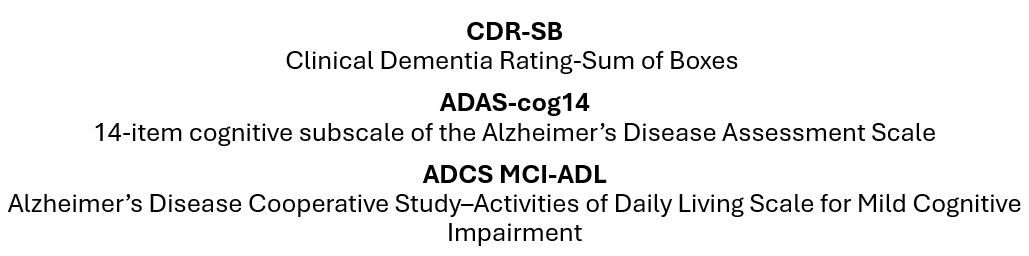
The latest data from the Clarity AD open label long-term extension (OLE) trial of lecanemab in adults with early-stage Alzheimer disease showed that among study participants who had low baseline levels of amyloid accumulation and received continuous lecanemab treatment for 3 years, nearly half (46%) either improved or showed no decline in symptoms and one-third (33%) showed improvement from baseline on the CDR-SB, a scale of global function and cognition, according to a news release from Eisai issued this morning.1
Similar findings were reported for performance on the ADAS-Cog14 measurement scale, according to an Eisai news release, with 46% of participants showing symptom improvement or no further decline and 43% showing improvement. The results were consistent for scores on the ADCS MCI-ADL, with half (51%) of the participants scored as improved or without decline (51%) and essentially half (48%) scored as showing improvement. Given the early stage of disease reflected by this group of Clarity AD participants, ie, with no or low tau (no tau/low tau) accumulation and low amyloid accumulation, the findings suggest that lecanemab treatment initiated earlier in adults diagnosed with AD "may have a positive impact on disease progression...and may provide continued benefits to patients with early AD over the long term," Eisai stated.1
These findings, along with other study outcomes, were presented at the 17th Clinical Trials for Alzheimer’s Disease Conference, October 29 to November 1, in Madrid, Spain.
Original Clarity AD
Eisai reported early results of the OLE following the original phase 3 Clarity AD trial of lecanemab at the July 2024Alzheimer's Association International Conference (AAIC).2 Findings presented during the meeting showed a mean change from baseline CDR-SB in participants treated with lecanemab of -0.45 at 18 months. The change doubled at 36 months, to -0.95, compared to "a prespecified natural history cohort of AD," the company said.2 The reduction in relative risk for progression to the next stage of disease severity was 30%. The findings from a Clarity AD substudy using tau positron-emission tomography (PET) were also presented at AAIC. The results showed that after 3 years of continuous treatment with lecanemab, more than half (59%) of the participants with no tau/low tau levels at baseline had improvement in symptoms or no decline and 51% experienced improvement from baseline on the CDR-SB scale.2
Investigators reported no new safety findings among Clarity AD participants treated with lecanemab over the 3-year OLE. Most amyloid-related imaging abnormalities (ARIA) were seen during the first 6 months of treatment with subsequent rates low and similar to ARIA rates observed among participants treated with placebo during the study's placebo-controlled phase.1 With regards to the incidence of ARIA by ApoEε4 status during the continuous treatment, the incidence was higher in ApoE4 homozygotes than in heterozygotes or non-carriers, but rates of new ARIA decreased after the completion of the 18-month core study as treatment continued, regardless of ApoEε4 status, according to the company statement.1
In June, the FDA accepted Eisai’s supplemental biologics license application for a monthly intravenous maintenance dosing of lecanemab, potentially allowing for more treatment flexibility. In the phase 2 and 3 studies, lecanemab was administered as a 10 mg/kg biweekly intravenous treatment, its approved indication. The FDA has set a Prescription Drug User Fee Act action date for January 25, 2025.2
Longer-Term Insights
Among a subcohort of 66 individuals participating in a phase 2 study of lecanemab as well as the phase 3 Clarity AD trial and chose to continue with the therapy, 13 received lecanemab for more than 5 years and 40 received treatment for more than 3 years. Among the latter group, more than half (15/24) remained in their initial stage of disease, Esiai stated.1 Responding to a treatment satisfaction survey, the 11 participants (or their caregivers) who were treated for more than 5 years responded with “very satisfied” or “satisfied” with regard to their lecanemab treatment. Moreover, between 45% and 73% responded that lecanemab treatment "frequently" or "very often" made them feel "more positive about their daily life, social activities, and memory.3
Preclinical Screening, Biomarkers
Eisai also reported an update on the company's phase 3 clinical study AHEAD 3-45, which has enrolled individuals assessed as having preclinical AD, ie, they exhibit no impairment clinically but show intermediate or elevated levels of brain amyloid.4
Potential study participants were screened using blood tests, cognitive function tests, amyloid PET scans, MRI, and tau PET scans. Based on amyloid PET results showing amount of Aβ accumulation in the brain, participants were assigned to 1 of 2 trials evaluating different dose levels of lecanemab: the A3 trial enrolled those with borderline Aβ levels in the brain, and those with positive Aβ levels were enrolled in the the A45 trial.
According to Eisai, the use of blood biomarkers, specifically the plasma Aβ42/40 ratio and p-tau217/tau217 ratio, for initial screening, significantly improved assessing eligibility of the cognitively intact participants for amyloid PET testing. Results of the blood test reduced the screening failure from more than 70% to less than 30%, Eisai stated. Plasma p-tau217 correlated particularly well with amyloid PET, suggesting it has a useful role as a biomarker for elevated brain amyloid. The AHEAD 3-45 trail completed enrollment in October.4
References
1. Eisai Presents Data on Benefits of Long-Term Administration of Dual-Acting Lecanemab at the 17th Clinical Trials for Alzheimer’s Disease (CTAD) Conference. News release. Eisai. October 31, 2024. Accessed October 31, 2024. https://www.eisai.com/news/2024/news202481.html
2. Halsey G. Lecanemab efficacy continues at 3 years of treatment for early Alzheimer disease. Patient Care. August 2, 2024. https://www.patientcareonline.com/view/lecanemab-efficacy-continues-at-3-years-of-treatment-for-early-alzheimer-disease
3. Watson D, Neam M, Stafford M, et al. Transitioning from Clinical Trial to Clinical Practice for Long-Term Lecanemab Treatment in Early Alzheimer's Disease: Perspectives from an Alzheimer's Disease Treatment Center. Poster presented at: Clinical Trials for Alzheimer's Disease; October 29-November 1, 2024. Madrid, Spain.
4. Sperling RA, Rissman B, Johnson KA, et al. Screening Plasma Biomarkers, Amyloid and Tau PET Imaging in the AHEAD 3-5 Study. Late breaking abstract presented at: Clinical Trials for Alzheimer's Disease; October 29-November 1, 2024. Madrid, Spain.
5. Rafi MS, Sperling RA, Donohue MC, et al. The AHEAD3-45 study: design of a prevention trial for Alzheimer's disease. Alzheimers Dement. 2023;19(4):1227-1233. doi:10.1002/alz.12748
Newsletter
Enhance your clinical practice with the Patient Care newsletter, offering the latest evidence-based guidelines, diagnostic insights, and treatment strategies for primary care physicians.