Updated Guidelines for Atrial Fibrillation from ACC/AHA Focus on Aggressive Prevention and Control and a Continuum of Care
The American College of Cardiology (ACC) and the American Heart Association (AHA) on November 30, 2023, released new guidance for prevention and optimal management of atrial fibrillation (AF).1
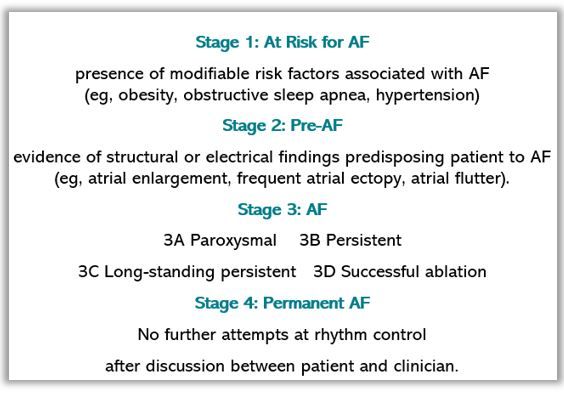
The guidelines, jointly published in the Journal of the American College of Cardiology and Circulation, for the first time provide a classification system for AF, the 4 stages reflecting the complexity of the condition and the need for a continuum of care that includes different strategies at different stages.
Other significant changes include a more prescriptive approach to lifestyle and risk factor modification to prevent the onset and progression of AF and recommendation for early and more aggressive rhythm control. The latter includes an upgraded recommendation for catheter ablation which now carries a Class 1 indication as first-line therapy for rhythm control in selected patients.1
“This is a complex disease. It’s not just an isolated disorder of the heart’s rhythm, and we now know that the longer someone is in AFib, the harder it is to get them back to normal sinus rhythm,” said Jose Joglar, MD, professor of cardiac electrophysiology at UT Southwestern Medical Center in Dallas and chair of the writing committee.2 “The new guideline reinforces the urgent need to approach AFib as a complex cardiovascular condition that requires disease prevention, risk factor modification, as well as optimizing therapies and patients’ access to care and ongoing, long-term management.”2
The guideline is the first comprehensive update on management of AF since 2014 and is based on a wide-ranging literature search performed between May and November 2022. The AHA and ACC collaborated with, and the publication is endorsed by the American College of Clinical Pharmacy and the Heart Rhythm Society.
Staging reflects disease progression1
The new staging classification (see Figure) replaces the previous focus on duration of arrhythmia which, according to the guideline authors, while it was useful, tended to prescribe intervention once AF had been diagnosed and focused more on specific therapeutic interventions. The revised paradigm recognizes AF as a progressive disease that requires tailored approaches at each stage and emphasizes prevention and screening to stratify risk early in the disease process.
The focus on a more aggressive approach to rhythm control stresses early restoration of sinus rhythm (SR) and continued management to help reduce AF disease burden. The ACC/AHA has assigned a Class 1 treatment recommendation for catheter ablation to restore SR in selected patients, typically those who are younger with few comorbidities, with symptomatic paroxysmal AF that does not respond to antiarrhythmic therapy. Recent evidence also demonstrates the superiority of catheter ablation over medication for SR restoration in persons with heart failure, prompting the ACC/AHA to upgrade the class of recommendation for this population as well. 1
“In the past, catheter ablation was considered a second line option after medications were tried and failed, and now we are advising that, in select AFib patients, you can proceed to catheter ablation as a first option,” Joglar said.2
Stroke risk, anticoagulation
The guideline preserves the recommendation for use of the CHA2DS2-VASc score to stratify risk for stroke and a subsequent choice for anticoagulation but encourages clinicians to include other risk variables and to use other risk prediction instruments to help clarify the approach when there is uncertainty. The more inclusive approach, the authors state, will improve prediction and also facilitate clinician-patient shared decision making.1
The class of recommendation for left atrial appendage occlusion devices also has been raised to a 2a based on additional data on safety and efficacy of the devices. Also based on a growing body of evidence for the role of data from wearable health trackers, the new guideline updates recommendations for “device-detected AF” that consider the interaction between duration of AF episode and the individual’s risk for thromboembolism.1
Similar to other chronic conditions, such as high blood pressure or type 2 diabetes, Joglar said we “now have a better understanding and more tools to prevent, treat and also mitigate the risk of AFib so that we can improve patient outcomes.”2
The writing committee was comprised of cardiologists, cardiac electrophysiologists, surgeons, pharmacists and patient representatives/lay stakeholders.1
References
Joglar JA, Chung MK, Armbruster AL, et al. 2023 ACC/AHA/ACCP/HRS Guideline for the Diagnosis and Management of Atrial Fibrillation: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. Published online November 30, 2023. doi: 10.1161/CIR.0000000000001193
Early rhythm control, lifestyle modification and more tailored stroke risk assessment are top goals in managing atrial fibrillation. News release. American Heart Association. November 30, 2023. Accessed November 30, 2023. https://newsroom.heart.org/news/early-rhythm-control-lifestyle-modification-and-more-tailored-stroke-risk-assessment-are-top-goals-in-managing-atrial-fibrillation
Newsletter
Enhance your clinical practice with the Patient Care newsletter, offering the latest evidence-based guidelines, diagnostic insights, and treatment strategies for primary care physicians.