Uptick in Food Allergy Not a Result of Increased Sensitization
Why has the number of food allergies increased but overall sensitization to food allergens remained static?
In spite of a recent large increase in the number of food allergies, sensitization to common food allergens did not increase over a recent two-decade span, according to a new study.
An analysis of blood samples taken from the late 1980s to the early 2000s from National Health and Nutrition Examination Survey (NHANES) data raises questions about increases in self-reporting of food allergies as well as emergency room visits and hospitalizations.
“Since the 1990s, studies have shown the prevalence of food allergies in children has grown by at least 50%,” said senior author Corinne A. Keet, MD, associate professor of pediatrics at the Johns Hopkins University School of Medicine. “Today, we think about 5% of children in the Unites States have a food allergy, with the most common triggering allergens found in milk, eggs, shellfish, and peanuts. Why allergies have seemed to increase, however, has been unclear and has led to a significant amount of research on causes underlying the food allergy ‘epidemic.'” The researchers say it remains “unclear whether these trends represent shifts in recognition of food allergy or in sensitization.”
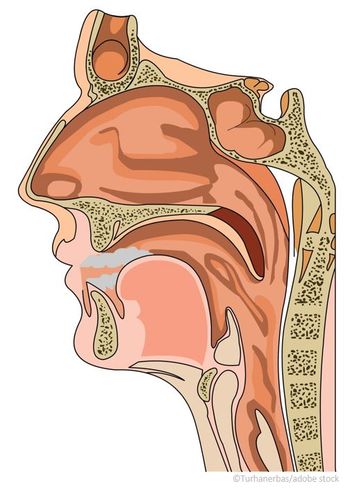
[[{"type":"media","view_mode":"media_crop","fid":"48301","attributes":{"alt":"","class":"media-image media-image-right","id":"media_crop_6948774562387","media_crop_h":"0","media_crop_image_style":"-1","media_crop_instance":"5756","media_crop_rotate":"0","media_crop_scale_h":"0","media_crop_scale_w":"0","media_crop_w":"0","media_crop_x":"0","media_crop_y":"0","style":"margin: 8px; float: right; width: 300px; height: 279px;","title":"©Alexander Chaikin/Shutterstock.com","typeof":"foaf:Image"}}]]The researchers measured food-specific immunoglobulin E (IgE) to peanut, milk, egg, and shrimp from subjects aged 6-19 years in the NHANES III from 1988-1994 (4995 subjects) and also in NHANES 2005-2006 (2901 subjects). Sensitization to foods was defined as overall, moderate-level, and high-level. Sensitization to individual and combined foods was compared between surveys, with analyses further stratified by race and/or ethnicity.
In NHANES III, the prevalence of food sensitization was 24.3% as compared with 21.6% in NHANES 2005-2006. There were no significant changes in the prevalence of any level of milk, egg, or peanut sensitization, but shrimp sensitization at all levels decreased markedly, the researchers noted.
Overall sensitization was 11.2 % in NHANES III versus 6.1% in NHANES 2005-2006.
There was a trend toward the increased prevalence of moderate- and high-level sensitization to the combination of milk, egg, and peanut among non-Hispanic blacks, but not other groups, they noted.
In conclusion, the researchers stated: “In contrast to our expectations, sensitization to common food allergens did not increase between the late 1980s/early 1990s and the mid-2000s among US 6-19-year-olds, and in fact decreased to shrimp.”
Keet said: “We were really very surprised. It’s important to know whether changing sensitization to foods underlies these trends because if sensitization hasn’t changed, then continuing to look for environmental factors that affect sensitization may not answer why food allergy has increased.”
More awareness of food allergies may be a possible explanation. “In the past, there may have been more people who just didn’t eat a food because it made them feel sick, but they didn’t necessarily call that an allergy. Today, we may be much more likely to suspect allergy when a child has a rash or other symptoms after eating a certain food,” said Keet.
Or possibly there has been a change over the past few decades in how food-specific IgE helps to trigger clinical food allergy, they suggested.
The researchers published their
Newsletter
Enhance your clinical practice with the Patient Care newsletter, offering the latest evidence-based guidelines, diagnostic insights, and treatment strategies for primary care physicians.