Data Review of Efficacy and Safety Study of Nirsevimab for RSV
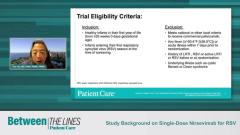
Tina Tan, MD, FAAP, FIDSA, FPIDS, and Flor M. Munoz, MD, MSc, discuss the initial efficacy data of the study on nirsevimab for Respiratory Syncytial Virus (RSV) and how it compared to placebo.
Episodes in this series

Transcript
Tina Tan, MD, FAAP, FIDSA, FPIDS: I think the major point that’s made here, when you look at the data that came out of the study, and you look at RSV-associated medically attended lower respiratory tract infection, we know that the vaccine efficacy value was around 75%. I think that is actually quite good, when you think about the amount of protection that we can provide these infants as well as the length of time that the infants are going to be protected. Then when you look at RSV-associated medically attended hospitalizations, they had an efficacy value of around 62% for the nirsevimab with regard to protection, which I think, again, really is a significant improvement in what we’re able to do now.
Flor M. Munoz, MD, MSc: If I could comment on that, as you have described, the objective was precisely to prevent RSV-associated [disease], so laboratory-confirmed more severe disease, [and] the measures to look at the severity of disease here were medically attended lower respiratory tract illness and hospitalization. The goal here, because of this monoclonal antibody’s long-acting capacity, was to do this long follow-up, as you mentioned, to be able to see protection in the first 6 months of life, so follow-up for at least 150 days, which is 5 months, and then a little bit past that to see if you could actually reduce that virus-specific lower respiratory tract illness in that period of time. As you’ve indicated, the objective of reducing medically attended lower respiratory tract illness, bronchiolitis pneumonia, of 70%, almost 75%, is quite impressive. You do see that this is a significant P value and confidence interval that goes between 50 [and] 87, basically comparing the cases that occurred in the treated group vs a placebo group. So [these] data [are] quite strong. I would comment regarding the hospitalization with an efficacy value that is a little bit lower of 62%, and in this case, the P value is a little bit over 0.05 with the confidence interval that goes into a negative as well. So, the comment here is that, yes, the trend is towards reduction of hospitalization as well. But I think that in this case, hospitalization, medically attended hospitalization, was not as a strong result as reducing the risk of medically attended lower respiratory tract illness.
Tina Tan, MD, FAAP, FIDSA, FPIDS: I think when you look at the time to event analysis for the medically attended RSV-associated lower respiratory tract infections, you can see quite clearly that those infants who got nirsevimab compared [with] those who got placebo definitely were much more protected compared [with] those who had placebo, when you’re looking at the proportion of infants who were free from having medically attended RSV[-associated] lower respiratory tract infections. We do know that nirsevimab does provide some, if not significant, protection against these infants getting those types of infection.
Transcript AI-generated and edited for clarity.
Newsletter
Enhance your clinical practice with the Patient Care newsletter, offering the latest evidence-based guidelines, diagnostic insights, and treatment strategies for primary care physicians.