
HIV and AIDS are becoming more common among people over 50, for many reasons. Providing adequate treatment can be a challenge. New guidelines are here to help.

HIV and AIDS are becoming more common among people over 50, for many reasons. Providing adequate treatment can be a challenge. New guidelines are here to help.

A 58-year-old man presented for care when he noticed a flat, dark area on his left upper arm. The lesion was set against a background of fairly severe photodamage. Family history was positive for melanoma (mother and 1 of 4 sisters). Click here for more details.

Whether Mom or infant takes the drugs, antiretrovirals during the first 6 months protect breast-fed infants against contracting HIV. In this interview, the lead author of the CDC-led study discusses the implications.

Many people with arthritis also have depression; this has been known for many years. Now it has been established that anxiety is even more common than depression among arthritis patients. Dr. Elizabeth Lin discusses why and how the mental health problem as well as the physical symptoms need to be addressed and resolved.

Anxiety is even more common than depression among people who have arthritis, a new study has shown. Here to discuss the implications for diagnosis and treatment is Eilzabeth Lin MD, a family medicine physician who is a longstanding researcher in the field of depression and pain.
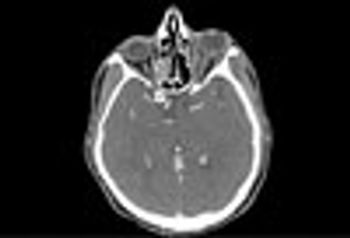
A 58-year-old man with a past medical history of chronic sinus disease and hypothyroidism presented with left periorbital pain and erythema that worsened despite outpatient treatment with topical antibiotics. An outpatient CT scan showed pansinusitis and orbital stranding. The diagnosis was orbital cellulitis and sinusitis.

Among the information of interest to primary care: Asymptomatic smokers may show signs of COPD, and what to do about it. How to treat obstructive sleep apnea as effectively as a sleep center. And things you may not know about inhalers.

A 16-year-old boy was complaining of pain in the maxillary left incisor/cuspid region. He had been experiencing discomfort for 1 year. He was otherwise healthy and a review of his other systems was unremarkable.

Obesity hypoventilation syndrome (OHS) shares clinical symptoms with obstructive sleep apnea (OSA) such as daytime sleepiness, headaches, and memory problems. Both the symptoms and their sequelae, however, can be much more severe in OHS. Here, guidance on what to look for and how to manage OHS.

The elderly patient has had type 2 diabetes for 15 years is now home bound after a stroke. Her HbA1c is 9.6 and she takes only metformin. Review the rest of her laboratory results and propose a management plan.

Red face. Roseacea? Lupus? Sunburn? No, it's seborrheic dermatitis. Here's how to tell.

There's no need to abandon abacavir as an option for AIDS treatment fearing adverse effects. This podcast features a new guideline that shows how to use easily ordered genetic tests to judge who can take the drug safely.


New guidelines on the use of antiretroviral therapy, together with recently published studies, highlight the benefits of early, short-term treatment on outcomes, clinical signs of the disease, morbidity and mortality, and secondary transmission.

Staff Salary Survey 2012 Here, you'll find detailed data on how much practices around the country are paying their various staffers.

A recent approval of an antiretroviral for children with HIV highlights the difficulties in treatment for pediatric HIV, which is not entirely eliminated in the US and tragically abundant elsewhere. It's also important for HIV among adolescents, which remains a concern in the US.


A panel of physiological markers of respiratory function adds significantly to the predictive value of clinical prognostic factors such as forced expiratory volume and age.
A new study that showed a link between a yearly dental x-ray and meningioma must have sent a shiver down many a spine. Here, oral medicine specialist Dr Jeff Burgess offers guidance about what to think, and how to respond when a concerned patient asks.

Despite widespread concern about the use of these drugs for patients with asthma and allergies, a review of the evidence shows that (used as recommended) there is very little risk from introducing a steroid into the upper respiratory system on a fairly regular basis, even for a child.