
All News


Contact stomatitis can occur as a result of cinnamon exposure. The condition can easily be managed by withdrawal of the antigen. A short course of systemic corticosteroid can produce dramatic improvement if symptoms are severe.

1. Giovannucci E, Stampfer MJ, Krithivas K, et al. The CAG repeat within the androgen receptor gene and its relationship to prostate cancer. Proc Natl Acad Sci USA 1997;94(7):3320-3323


For the past 20 years, I have been visiting developing nations to deliver healthcare. Recently, I made a conscious decision to look for a case of child abuse to write about. Late in 2011, during one of my visits to a third world country, I encountered multiple situations that rose to the level of possible child abuse. Here, I describe 3 such cases.


Is obesity really leading to an increase in GERD? Or, has GERD just become a catch-all phrase for all sorts of upper GI distress? Has GERD become the new "dyspepsia"? G. Richard Locke, MD, FACG, from the Mayo Clinic, Rochester, MN, discusses his findings as presented at the ACG 2011 program.

A 52-year-old woman presents with severe intra-oral ulceration and oral pain. She reports that several years earlier, she had been taking cephalexin when severe intra-oral ulceration developed.

Prevalence for overweight (BMI 24.9 to 29.9) and obesity (BMI > 30) have been steadily rising for the past 30 years-two-thirds of Americans now qualify as overweight or heavier. Hypertension, hyperlipidemia, coronary artery disease, type 2 diabetes, sleep apnea, and GERD prevalence are following this epidemic. Obesity is now the second most common preventable cause of death, exceeded only by smoking.

Compare your salary, bonus structure, overhead ratio, and career plans with those of your peers, using this exclusive research by ConsultantLive

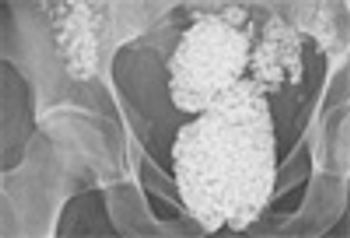
Gout, once considered a disease of kings, is now a common and equal opportunity disease that affects as many as 3 million people in the US. Gouty arthritis has now become a serious problem in organ transplant recipients; in diuretic users; and in patients with CKD, hypertension, metabolic syndrome, heart failure, plus more.


Advertising InformationClick here to view our Media Kit Brett Baxter, Director of Digital Business DevelopmentBrett.Baxter@UBM.com or call 201-984-6271.

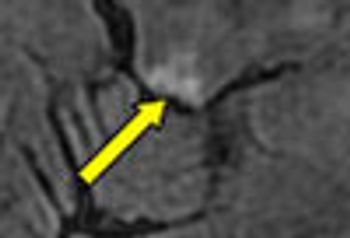
A 76-year-old man presented with left-sided chest pain, after a fall. He had tenderness along the left 8th rib and left basal rales. CXR showed non-displaced fractures of the 7th and 8th ribs with a small effusion and a right postero-basal rounded opacity.

A 71-year-old man was admitted to the MICU for weaning from mechanical ventilation. The history revealed a global decline over the previous 3 to 4 weeks predominated by cognitive impairment, mood swings, somnolence, and limb weakness. No respiratory symptoms were noted.

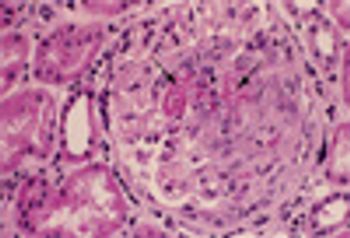
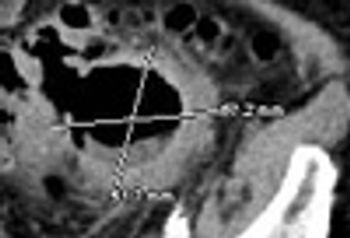
A 56-year-old was seen in the ED after 4 days of hemoptysis and intermittent left chest pain. He also complained of exertional dyspnea and arthralgias. He had been treated for “pneumonia” twice during the past month. Histories were unremarkable.
