Articles by Sonia Arunabh, MD
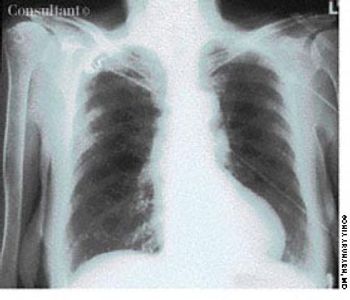
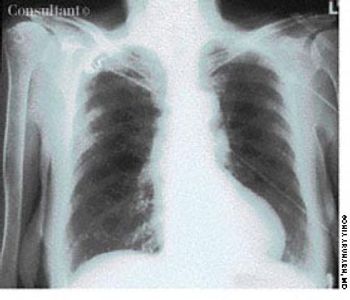
A 40-year-old man, originally an Ohio resident, underwent a chest x-ray study during medical clearance following surgery to repair a hernia. Although the patient had no pulmonary symptoms, the film showed multiple small, punctate calcifications in both lung fields.
A 72-year-old nursing home resident was hospitalized with fever, chills, and rigors of 2 days' duration. The nursing home staff reported the patient had dysphagia after a recent stroke.

A 42-year-old woman complained of facial puffiness, fullness, and redness for 2 weeks, which were gradually becoming more severe. She also noticed a sensation of “heaviness” in her head. The patient had no significant past medical history. She denied having a cough, shortness of breath, hoarseness, allergies of any kind, and neurologic deficits. Her weight and appetite were unchanged. She had smoked a pack of cigarettes every day for the past 20 years.

The significant palmar erythema seen on the hands of a 60-year-old man with alcoholic cirrhosis is a sign of underlying chronic liver failure.

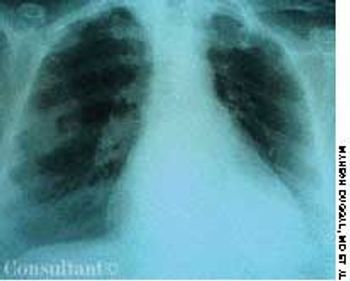
A 72-year-old woman who was being evaluated for medical clearance for an elective cholecystectomy was asymptomatic, except for biliary colic. She had had pulmonary tuberculosis (TB) 40 years earlier, for which she had undergone surgery on the right hemithorax-a fact borne out by a thoracotomy scar. An x-ray film of her chest, shown here, demonstrates numerous plastic balls in the right thoracic cavity. This is an example of collapse therapy for pulmonary TB, which was practiced years ago, before the availability of effective antituberculous medications.

Bilateral swelling and pain of the distal interphalangeal (DIP) joints for several months brought this 65-year-old woman to her physician. She complained also of stiffness in the region of the DIP joints when she arose in the morning and after short periods (less than 15 minutes) of inactivity. A history such as this, in conjunction with the appearance of the patient's hand, is typical of Heberden nodes, which are a manifestation of osteoarthritis (OA).

A 65-year-old man was hospitalized with dyspnea and fever of a few days' duration. He complained of excessive malaise, fatigue, and weight loss but denied any hemoptysis. The patient had a history of alcohol abuse.

During the past few months, a 50-year-old woman had experienced cough, dyspnea, mild hemoptysis, and a 30-lb weight loss. She had no fever, chills, or rigors. The patient had smoked cigarettes for 30 years.

A 67-year-old man with a 5-month history of cough, shortness of breath, and pain in the left anterior chest wall sought medical evaluation. The patient denied fever, chills, and hemoptysis. He reported a recent weight loss of 25 lb. The patient had smoked cigarettes for 37 years.

A 48-year-old man complained of difficulty in swallowing both solid food and liquids. The dysphagia began several years earlier and had become increasingly severe and more frequent over the past 2 to 3 years. Vague heartburn without reflux and frequent regurgitation were also troublesome.
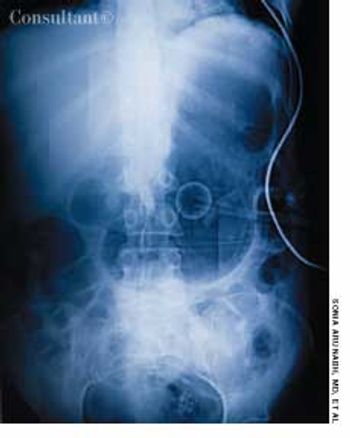
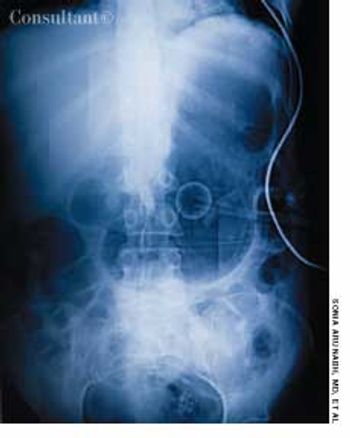
A 70-year-old man was brought from a nursing home to the emergency department with abdominal distention and vomiting of recent onset and a 2-day history of fever and abdominal pain. The patient had chronic obstructive pulmonary disease, type 2 diabetes mellitus, and hypertension. His gastric feeding tube, which had been placed via percutaneous endoscopic gastrostomy, was blocked.

These painful eczematous lesionsat the angle of the mouth and thebase of the nostrils had been presentin a 52-year-old woman for 3days (A). Some of the vesicles hadulcerated and left a crust over theregion. The patient said she had hadsimilar attacks in the past. The diagnosisof recurrent herpes simplexvirus 1 (HSV-1) infection was made.The patient was treated with acyclovirfor 1 week, and all the lesionsdisappeared.

A 40-year-old man presented with a 1-year history of progressively worsening dysphagia. He reported difficulty in swallowing both solids and liquids and had experienced mild weight loss during the past few months. He had no history of gastroesophageal reflux.

Bilateral swelling and pain in the distal interphalangeal (DIP) joints for severalmonths brought this 65-year-old woman to her physician. She complained alsoof stiffness in the region of the DIP joints when she arose in the morning andafter short periods (less than 15 minutes) of inactivity. A history such as this,in conjunction with the appearance of the patient’s hand, is typical of Heberdennodes, which are a manifestation of osteoarthritis (OA).

An 85-year-old man was admitted to the hospital with acough and shortness of breath of 1 week’s duration anda fever and increased sputum production for 2 days. Hishistory included renal cell carcinoma and metastatic renalcancer for 2 years. The patient had smoked cigarettesfor 30 years. He had lost 30 lb during the last few months.A chest film revealed pneumonia of the right lowerlobe. Metastatic nodules were noted on the scalp; extensivelung, bone, and brain metastases also were found.

A 48-year-old woman was admitted to the hospital with deep venous thrombosis of the right leg. She had a history of non-Hodgkin lymphoma, which was in remission. The patient had been a heavy smoker for many years.

A 64-year-old woman with a history of diabetes, hypertension, and lymphoma was admitted to the hospital with a dull headache, conjunctival congestion, and slight dyspnea. Her pulse rate was 96 beats per minute; blood pressure, 146/68 mm Hg; and respiration rate, 22 breaths per minute. She also had increased jugular venous distention; cardiovascular and chest examination findings were normal. Edema of both arms and dilated blood vessels on the anterior chest wall were noted.

A 72-year-old woman presented for her annual physical examination. She had been treated for tuberculosis 20 years earlier. The patient did not smoke cigarettes; she denied fever, chills, and rigors.