Articles by Sonia Arunabh, MD

A 52-year-old woman was admitted tothe hospital with progressive shortnessof breath of 2 days’ duration. Bronchialasthma had been diagnosed 6 monthsearlier; inhaled corticosteroids, bronchodilators,and leukotriene antagonistswere prescribed. Despite aggressivetreatment, the patient’s dyspneaand wheezing worsened.

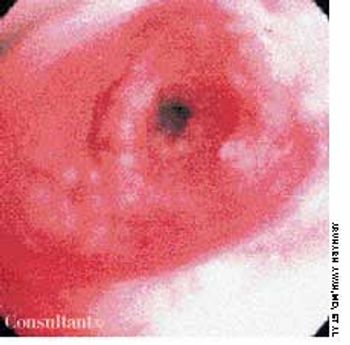
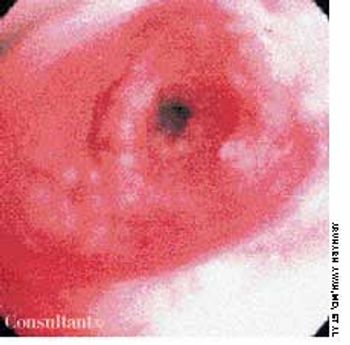
A 72-year-old morbidly obese man who had diabetes mellitus was admitted to the hospital from a nursing home with a fever of 4 days' duration. A tracheostomy had been performed 3 months earlier for respiratory failure. The patient was being treated with corticosteroids for chronic obstructive pulmonary disease.
A 2-month history of cough sent a 62-year-old woman for medical evaluation. The patient denied fever, chills, and rigors but reported seeing streaks of blood in her sputum during the past month. The patient had undergone a right nephrectomy 4 years earlier for renal cell carcinoma.
A 72-year-old woman presented for her annual physical examination. She had been treated for tuberculosis 20 years earlier. The patient did not smoke cigarettes; she denied fever, chills, and rigors.
Having suffered progressive shortness of breath for 2 years, a 35-year-old man was eventually hospitalized. The patient's dyspnea had worsened over the past year, but he had neither chest pain nor palpitations. His primary care physician first noticed finger clubbing 8 months ago.

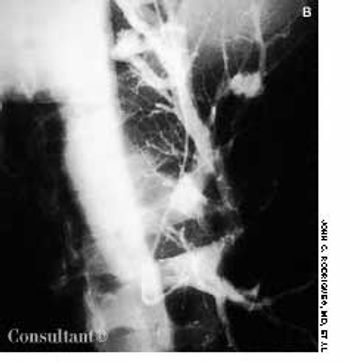
A 69-year-old woman was admitted to the hospital with wheezing and dyspnea. She also complained of hoarseness and slight dysphagia that had caused a loss of 12 lb during the past 4 months. The patient had been treated for bronchial asthma as an outpatient, but the worsening episodes of wheezing were not being controlled by bronchodilator therapy.

Over the past 6 months, a 72-year-old man was troubled by a persistent cough; he also had lost 9 kg (20 lb). He had no fever or chills, but he noticed mild streaking of blood in his sputum during the past month. He had been a cigarette smoker for 50 years.
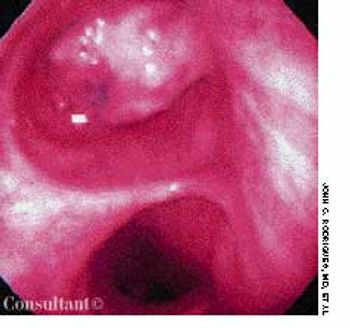
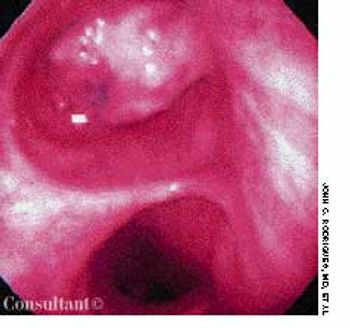
Persistent collapse of the right lung led to hospitalization of a 62-year-old woman with a history of colon cancer. She had no fever, chills, rigor, or hemoptysis. The patient underwent bronchoscopy to rule out any central endobronchial obstructing lesion.

For the past 6 weeks, a 72-year-old woman with a history of ovarian cancer had had intensifying dyspnea. Initially, she thought her breathing problem was caused by progressive congestive heart failure.

A 73-year-old man was admitted to the hospital with pain in his hands, feet, and elbows. The patient, an alcoholic, had a 20-year history of hypertension and diabetes. Deformities of the hands and feet had developed during the past 5 years. Tophi were present over both ear lobes. The serum uric acid level was 15 mg/dL.

A 48-year-old woman was admitted to the hospital with deep venous thrombosis of the right leg. She had a history of non-Hodgkin lymphoma, which was in remission. The patient had been a heavy smoker for many years.

A 64-year-old woman with a history of diabetes, hypertension, and lymphoma was admitted to the hospital with a dull headache, conjunctival congestion, and slight dyspnea. Her pulse rate was 96 beats per minute; blood pressure, 146/68 mm Hg; and respiration rate, 22 breaths per minute. She also had increased jugular venous distention; cardiovascular and chest examination findings were normal. Edema of both arms and dilated blood vessels on the anterior chest wall were noted.

Painful eczematous lesions at the angle of her mouth and the base of her nostrils had been bothering a 52-year-old woman for 3 days. Some of the vesicles had ulcerated and left a crust over the region. The patient said she had had similar attacks in the past. The diagnosis of recurrent herpes simplex virus 1 (HSV 1) infection was made. The patient was treated with acyclovir for 1 week, and all the lesions disappeared.

A 55-year-old man complaining of backache had localized tenderness at the paraspinal region over the posterior portion of the right 7th rib. A CT scan of the thorax revealed erosion of this portion of the rib, along with a space-occupying lesion that displaced the adjacent pleura and lung. Needle aspiration and biopsy study of this mass showed it to be a plasmacytoma.
A 40-year-old man was being treated as an outpatient with inhaled corticosteroids and bronchodilators for a presumed diagnosis of bronchial asthma. Worsening episodes of shortness of breath during the past few months sent him to the emergency department for a second opinion.

For 1 month, an 82-year-old woman had had episodes of coughing. Chronic bronchitis had been diagnosed; however, antibiotics and bronchodilators failed to control symptoms.

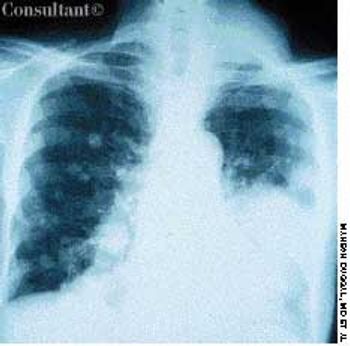
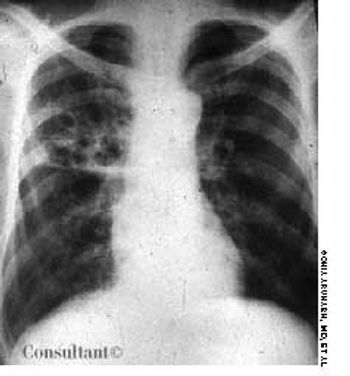
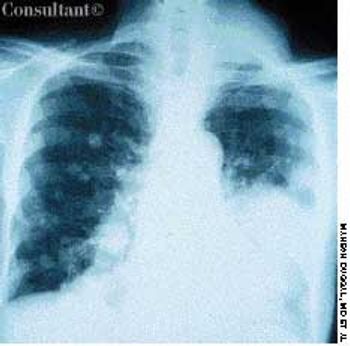
A 30-year-old man, who was homeless, was admitted to the hospital with a several-month history of dyspnea and fever. He complained of producing excessive sputum and having frequent bouts of hemoptysis. Bilateral crackles were heard during examination of the lungs. The patient was in acute respiratory distress and was intubated to provide ventilatory support.
A 60-year-old comatose man was brought to the emergency department (ED). He had a history of diabetes, hypertension, and alcohol abuse. Relatives reported that the patient was noncompliant with his antihypertensive medication regimen.

For the past few days, a 75-year-old man with a history of chronic obstructive pulmonary disease had suffered from dyspnea and fever (temperature, 38.3°C [101°F]). He also complained of producing excessive foul-smelling sputum but denied any hemoptysis.

A 60-year-old woman with a 3-month history of cough, chest pain, and shortness of breath was brought to the emergency department. The patient denied any history of fever, chills, or rigors; she complained of mild hemoptysis for 1 week and a 9-kg (20-lb) weight loss during the last few months. The patient had smoked cigarettes for 40 years.

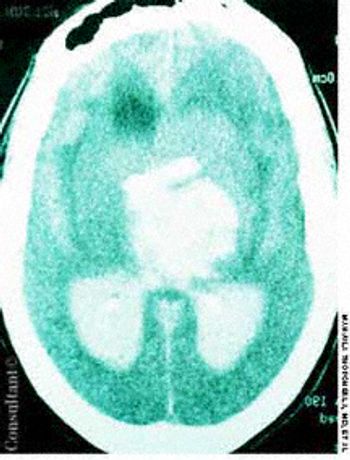
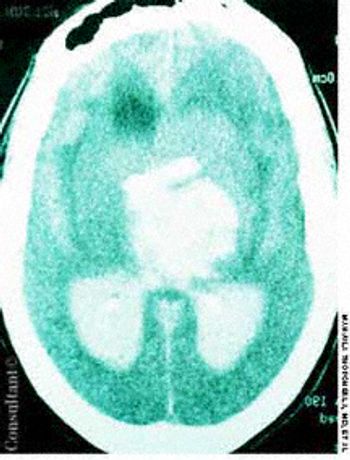
A 30-year-old man presented to the emergency department with new-onset seizures. His past medical history included loss of vision for 1 year, deafness, and osteomyelitis of the mandible.

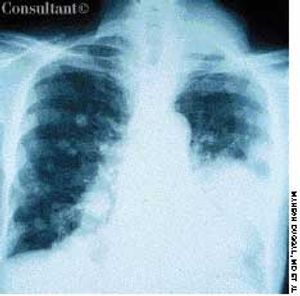
A 25-year-old man, who was an injection drug user, presented with a several-day history of dyspnea and fever. He complained of excessive malaise, fatigue, and weight loss but denied any hemoptysis. The examination of the lung revealed bilateral crackles in both lower zones.
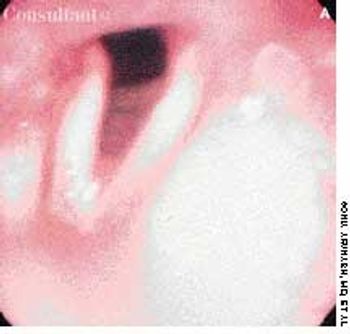
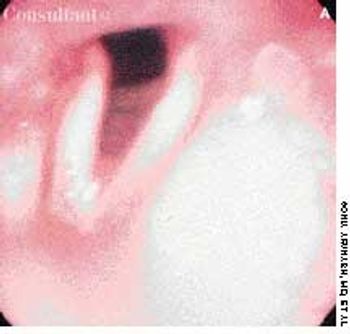
A 67-year-old man had been hoarse since undergoing a thyroidectomy for carcinoma nearly 3 months ago. Indirect laryngoscopy now confirmed paralysis of the right vocal cord, which was fixed in the paramedian position. The left vocal cord appeared normal.

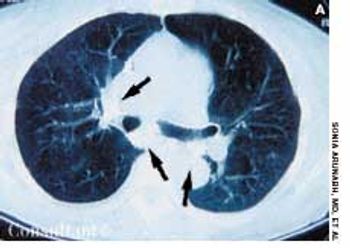
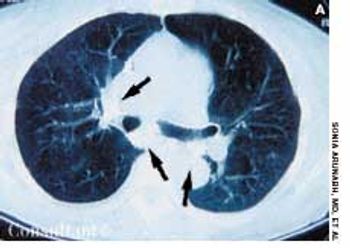
A 52-year-old woman who was undergoing chemotherapy for lymphoma was admitted to the hospital with fever of a few days' duration. The patient had smoked cigarettes for many years; she had no history of deep venous thrombosis.
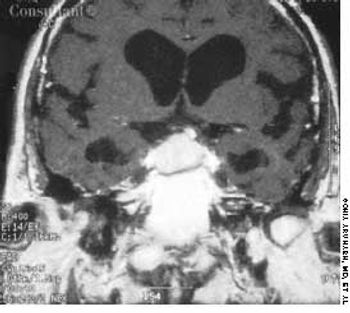
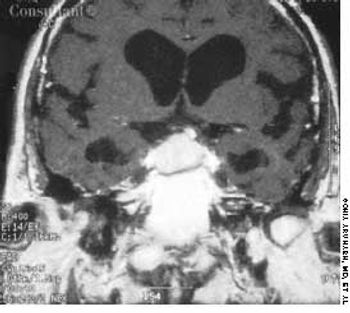
A 40-year-old woman with a history of amenorrhea complained of recent headaches and galactorrhea for the last 6 months. A neurologic work-up revealed bitemporal hemianopia, and a radiograph of the skull suggested an enlarged sella turcica. A large pituitary adenoma disclosed by an MRI and a serum prolactin level of 360 µg/L led to a diagnosis of prolactinoma.

A mass on the right side of her face-over the right parotid region-had been growing for the past 4 years, according to this 65-year-old woman. There was no evidence of facial nerve involvement.
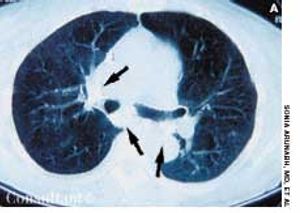
Having been treated for pulmonary tuberculosis (TB) 25 years earlier, a 60-year-old man (a nonsmoker) now complained of a chronic cough. The cough was occasionally accompanied by yellowish sputum but no hemoptysis. Examination revealed persistent coarse crackles in the right posterior hemithorax, and the x-ray study seen here established the diagnosis of cystic bronchiectasis.

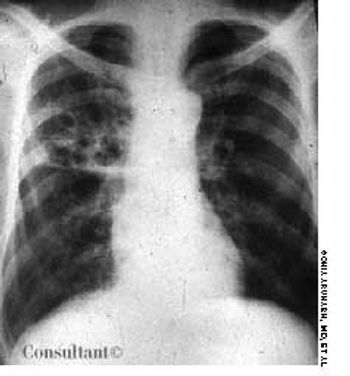
An 85-year-old man was admitted to the hospital with a cough and shortness of breath of 1 week's duration and a fever and increased sputum production for 2 days. His history included renal cell carcinoma and metastatic renal cancer for 2 years. The patient had smoked cigarettes for 30 years. He had lost 30 lb during the last few months.
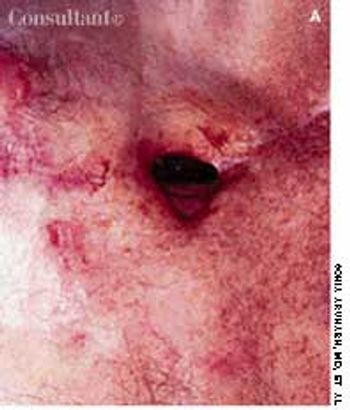
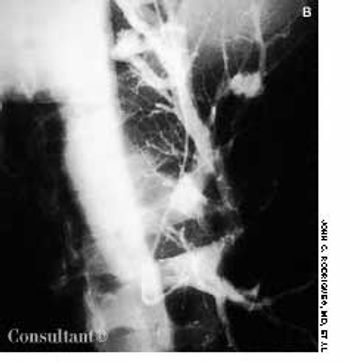
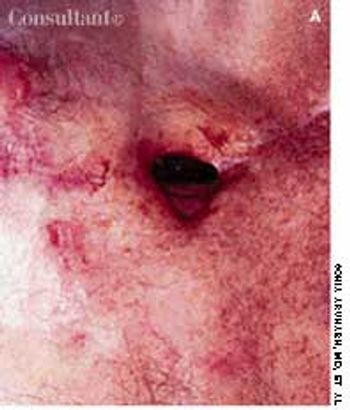
An 82-year-old man underwent right pneumonectomy for squamous cell carcinoma of the right lower lobe. His postoperative course was complicated by prolonged air leak from the chest tube, suggesting a bronchopleural fistula secondary to leakage from the bronchial stump. Over the ensuing 3 months, the air leak slowly decreased, but the patient was left with a nonhealing scar on the anterior thoracic cavity, as seen here.

A 42-year-old woman came to the emergency department because of hematuria for 1 day, a low-grade fever, and weight loss over the past 2 months. She denied having any abdominal pain or urinary problems. Pallor was the only noteworthy physical finding.