The 35-year-old man is a new patient for you. He says he was given Vicodin when he had a similar injury a number of years ago. How do you proceed?
The 35-year-old man is a new patient for you. He says he was given Vicodin when he had a similar injury a number of years ago. How do you proceed?

When are antiviral drugs appropriate to treat "shingles" and what is the first-line treatment for post-infection pain?
Opioids, imaging, and constipation-try this trio of questions on issues related to pain management.
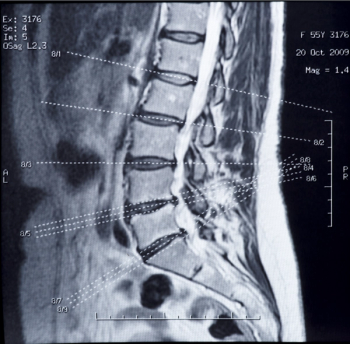
Low back pain is one of the most common reasons patients seek primary care; 3 new studies confirm what most of them don’t want to hear: less treatment is better than more.

Up to 50% of patients taking opioids for an extended period develop constipation. Patient education and basic prevention can help mitigate the side effect.

An estimated 10% to 20% of women experience major depression during pregnancy. Opioids could double that trouble.

Best practices make a strong case against prescribing benzodiazepines for chronic pain patients taking opioids. But are we following best practices?

A new study found that alcohol was involved in more than 20% of both opioid- and benzodiazepine-related deaths reported to the Drug Abuse Warning Network in 2010.

Difficulty with sleep is a common problem for people with chronic pain. Plus, it is well known that while pain medications cause sedation, they can also disrupt normal sleep cycles.

Deaths from opioid overdoses routinely claim headlines but nearly as many fatalities are caused each year by nonsteroidal anti-inflammatory drugs. Who's tracking trouble under the radar?

The results of several recent studies on both drug classes may come as a surprise. Will they change the way you prescribe either or both for pain?

The answer to this question has long been considered to be, "yes" and for what seem to be logical reasons related to the nature of chronic pain. But, where's the science to support the belief?

Three new opioid analgesics that purport to offer benefits that current products lack come with marketing messages that ring both contradictory and redundant.

Controversy around FDA approval of an extended-release formulation of the opioid hydrocodone includes well-founded concerns about abuse but also exposes enduring ignorance about opioid analgesics in general.

Pain may be an ongoing problem even after successful treatment for cancer; effective pain management, however, may be overlooked.

The hydrocodone/acetaminophen combination is moved to Schedule II from III while single-agent extended-release hydrodocone is approved without a tamper-resistant mechanism.

The use of general anesthesia to speed opioid detox without the discomforts of withdrawal has no scientific support.

New opioid labeling restricts the type of patient who should be prescribed long-acting/extended release formulations.

Guideline recommendations are not only frequently being ignored, but the number of physicians not using them is growing.

The current study may help create new pathways for better understanding and developing more effective and more specific medications.

Rotating opioids can reduce the risk of developing tolerance to the analgesic effects of any single drug and of developing hyperalgesia.

"The patient's report" has long been considered the most valid measure of human pain. Can fMRI replace that?

CRPS is essentially a clinical diagnosis. Allodynia and hyperalgesia are notable criteria for the diagnosis for type 1 and type 2.

CRPS may involve central and peripheral factors, the latter including an inflammatory process, peripheral sensitization, and changes in sodium channels.

Steroid injections for low back pain, tennis elbow, provide acute relief, but perhaps long-term damage.

Opioid medication prescriptions in emergency departments should be limited to a 3-day supply.

Epidural steroid injections turned deadly raise pointed controversy over poor oversight of compounding pharmacies. But tainted or not, are the injections a valid therapy for back pain at all? Here, one expert’s opinion.

Chronic pain patients may benefit from dietary modifications including changes in the amounts of PUFAs, polyamines, and flavonoid-rich foods they eat.

The Screener and Opioid Assessment for Patients with Pain-Revised and Current Opioid Misuse Measure are used to assess the risk of abuse of opioid analgesics.

The Risk Evaluation and Mitigation Strategy program for extended-release and long-acting opioids may not mitigate illegitimate prescribing.