
On This Page • Diabetes Q&A • Images in Diabetes • Juvenile Diabetes • Diabetes and Mental Health • Guidelines and Recommendations • News • Patient Resources • Tools

On This Page • Diabetes Q&A • Images in Diabetes • Juvenile Diabetes • Diabetes and Mental Health • Guidelines and Recommendations • News • Patient Resources • Tools



Glycemic Control and Type 2 Diabetes Mellitus: The Optimal Hemoglobin A1c Targets. A Guidance Statement from the American College of Physicians

Diabetes is one of the most common and most challenging diseases in primary care. How best to help your patients achieve glycemic control? To that end, we have created this resource page.

To save time and minimize pain and tissue trauma when injecting a joint or soft tissue with a corticosteroid, use a single needle and 2 screw-on syringes. Fill the first syringe with lidocaine and the second with the corticosteroid, then lightly but securely attach the first syringe to the needle. After inserting the needle and achieving local analgesia in the desired location, simply leave the needle in place and, while holding it firmly, switch the syringes; then inject the corticosteroid.

Practical Pointers

During circumcision, a newborn is noted to have continuous dribbling of urine from his meatus and stool from his anus. After several minutes of observation, the urinary stream appears weak and remains a constant trickle. The baby boy was born at term via an uncomplicated spontaneous vaginal delivery. He was treated in the neonatal ICU for hypoglycemia. A radiograph of his pelvis is shown.

Questions from parents touch on almost every aspect of child-rearing and can pose some of the greatest challenges in daily practice. Here, help with some of the thornier questions parents ask.

Specialty formulary management strategies, ePrescribing, and unique formulary benefit designs top the list of critical initiatives at MCOs, according to Cynthia J. Pigg, RPh, MHA, executive director of the Foundation for Managed Care Pharmacy. She discusses results from the Foundation’s 2009 Emerging Trends Survey.

It’s quick, easy and free to register on Consultantlive.com. Your first membership benefit: enter a drawing for an Amazon Kindle! Registered users also get unlimited access to everything our site has to offer, including the ability to print and share content, premium content, and clinical updates sent right to your in-box.
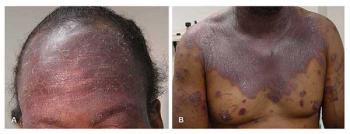
A 50-year-old African American man with HIV infection had a CD4+ T-cell count of 18/μL (1%), CD8+ cell count of 1035/μL (69%), and CD4:CD8 ratio of 0.01 at the time of diagnosis. He had multiple erythematosquamous skin lesions over his forehead, face, chest, back, and extremities

In 2006, the CDC recommended “opt-out” routine HIV testing in all health care encounters for persons 13 to 64 years of age. While this recommendation has garnered some support, concerns about the feasibility of such routine testing in a busy office without disrupting patient care has persisted. We report the results of a pilot study to determine the feasibility of routine testing in a busy urban clinic.

Hear an interview with Ted Rosen, MD, professor of dermatology at Baylor College of Medicine, and chief of Dermatology Service at Veterans Affairs Medical Center, Houston. Dr Rosen has a keen interest in current healthcare reform; he recently attended a summit in Washington with a group of think-tank leaders who are at the forefront of reform efforts.




