
Those least likely to schedule further screening mammograms had received a false-positive with recommendation for follow-up after only a short interval.

After a False Positive Result, Screening Mammography May Not be a Priority for Some Women

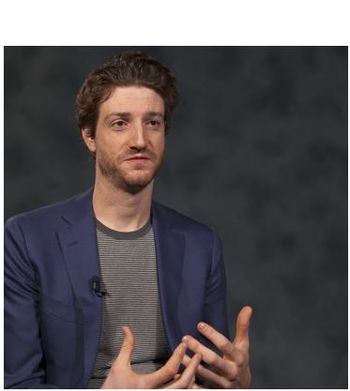
Researcher Explains How Women Respond to a False Positive Breast Cancer Screening Result

Those least likely to schedule further screening mammograms had received a false-positive with recommendation for follow-up after only a short interval.

Regulations have been amended under the Mammography Quality Standards Act of 1992 to ensure women receive quality mammography for early breast cancer detection and prevention.

Your daily dose of the clinical news you may have missed.
GLP-1RAs were associated with a significantly reduced risk of obesity-associated cancers including gallbladder cancer, pancreatic cancer, and meningioma.
Get a quick overview of recommendations for preventive health services and screenings focused on the unique needs of women across the lifespan.
Over 4 million cancer deaths have been reverted since 1991, but new cancer cases are estimated to reach over 2 million, according to new data from an annual American Cancer Society report.

Your daily dose of the clinical news you may have missed.

In postmenopausal women with HR+ breast cancer who had obesity, recurrence of breast cancer while on aromatase inhibitor therapy was 18%, report investigators.

Women's Health Week (May 14-20, 2023) is an ideal opportunity to review the top research, policy shifts, and potential drug approvals that affect your patient panel.

The lower recommended starting age for screening reflects rising cancer diagnoses among younger women and persistently high mortality rates among Black women.

A combination of outreach measures tailored to the needs of rural Midwest women increased recommended screenings by as much as 6-fold.

Race- and ethnicity-specific starting ages for screening would help prevent early breast cancer mortality among Black women, according to authors of a new study.
Breast cancer survivors rely on their primary care clinicians as resources integral to their recovery and return to optimal function. Physiatrist Sean Smith, MD, offers details.
In this Medical News Minute, Dr Bobby Lazzara reviews a study on the influence of media bias on far-reaching medical decisions in the general public.

October is Breast Cancer Awareness Month and Pregnancy and Infant Loss Awareness Month. Check here for a brief roundup of the latest women’s health news.

Women who exercise may lower their risk, although those who have received hormone replacement therapy may not get the same benefit. Organized programs can help.

Outcomes are poorer for young women and others with breast cancer when blood sugar levels reflect prediabetes or undiagnosed diabetes. What can you do?

We see survivors of breast cancer in primary care practice every day. Here, 8 guideline recommendations to help you ensure their continued health.

This case highlights medication errors that can result from drug interactions noted with the use of tamoxifen or other chemotherapeutic agents.

ROCKVILLE, Md. -- The FDA has approved the osteoporosis drug raloxifene (Evista) for prevention of invasive breast cancer in high-risk or osteoporotic postmenopausal women.

A 51-year-old woman has had a progressiverash on the trunk, proximalarms, and legs for 2 weeks, followingthe latest round of chemotherapy forbreast cancer. Around the time thatthe rash erupted, she was also takinglevofloxacin for a productive cough.Cutaneous lupus erythematosus wasdiagnosed years ago, but she hasbeen disease-free for the past 5 years.Chemotherapy is being withheldpending diagnosis of the rash.

A 73-year-old man is admittedto the hospital with pulmonary tuberculosis.A 3-drug fixed combination-isoniazid, rifampicin, and pyrazinamide-and ethambutol are given.Within an hour, a global urticarialrash erupts (A and B).

For 2 weeks, a 58-year-old woman has experienced increasingfatigue with activity. She has needed to nap duringthe day, has not been able to perform her usual activities,and has missed 3 days of work. She also complains of“muscle aches”-mainly in her back. She denies headache,dyspnea, fever, hot or cold intolerance, and alteredmentation.

Any discussion of theutility and reliabilityof mammography mustfocus on what is good forindividual patients-not onwhat the results of a Europeanpublic health researchproject have determined isgood for society as a whole.What is good for most patientsis annual screeningmammography beginningat age 40 years (and for patientsat very high risk forbreast cancer, mammogramsbeginning much earlier,and possibly performedmore frequentlythan once a year).1

The scientific literatureon screeningmammography can be confounding.This poses a continuingdilemma for bothpatients and clinicians. Nevertheless,objective analysisof the available data canprovide reasonable guidelinesfor the primary careclinician who must decidewhether screening mammographyhas benefit foran individual patient.