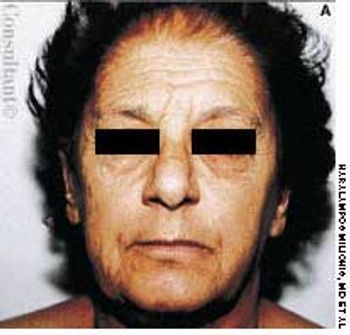
A 79-year-old nursing home resident was hospitalized for evaluation of hyperkalemia and leukocytosis. Her medical history included hypertension, respiratory failure with subsequent tracheostomy placement and ventilator dependency, and anemia. Both of her legs had been amputated above the knee secondary to complications of type 2 diabetes mellitus.