
A boy was born to a gravida 2, para 1, 26-year-old woman at 37 weeks' gestation. The pregnancy had been complicated by gestational diabetes.

A boy was born to a gravida 2, para 1, 26-year-old woman at 37 weeks' gestation. The pregnancy had been complicated by gestational diabetes.
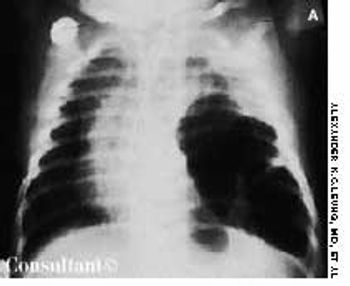
An irritable, lethargic, toxic-looking, and slightly cyanotic 2-month-old boy had a temperature of 40°C (104°F), malaise, and a cough for 2 days. The infant's heart rate was 98 beats per minute, and his respiratory rate was 55 breaths per minute. He had nasal flaring, sternal and subcostal retractions, diminished breath sounds, and scattered rales over the left lung, which was dull to percussion.

A 10-year-old boy presented with a 6-month history of a painless mass on the left side of the scrotum. The overlying skin had a bluish discoloration. The mass felt like a “bag of worms.” When the boy stood, venous varicosity could be palpated along the spermatic cord. This venous distention increased when he performed Valsalva's maneuver and decreased when he was recumbent.

A 40-year-old man requested evaluation of several cherry-red papules, which he had noticed on the upper part of his trunk for the past 12 months. The eruptions were diagnosed as cherry angiomas, also known as Campbell de Morgan spots.

Severe pain in the scrotum during a soccer game sent a 14-year-old boy to his physician. The right testicle was swollen and exquisitely tender. On exploration, it was hemorrhagic and blue-black. A small incision in the tunica of the testis revealed arterial bleeding, which indicated that the testis was still viable. The right testicle was untwisted and fixed to the scrotum.

A pruritic, erythematous rash developed in a 6-year-old boy over the previous 5 days. The rash erupted in crops; the lesions appeared initially as rose-colored macules, progressed rapidly to papules and vesicles, and finally crusted. The distribution of the lesions-with the greatest concentration on the trunk-is typical of chickenpox.

When this boy was born, he was covered by a transparent membrane resembling oiled parchment or collodion. The membrane was shed within 2 weeks and, subsequently, the infant was found to have normal skin. Lamellar ichthyosis usually develops in babies with this condition, although in some the skin clears completely.

A 37-year-old man presented with a reddish nodule in the umbilical area that had been present since early infancy. The lesion had been cauterized with silver nitrate several times in the past but had not resolved. No drainage or secondary infection was noted, and the patient was otherwise in good health.

At 3 days of age, this infant was noted to have an erythematous, maculopapular rash on the face, chest, abdomen, and back that included some pustule-like lesions.

Also known as congenital aganglionic megacolon, this condition is characterized by a congenital absence of ganglion cells in the submucosal (Meissner) plexus and the myenteric (Auerbach) plexus in one or more segments of the colon. This is attributable to a failure of migration of nerve cell elements from the neural crest in a cephalocaudal direction along the GI tract. The absence of parasympathetic innervation causes failure of relaxation of the internal anal sphincter. An aganglionic colon does not permit normal peristalsis to occur and thus results in a functional obstruction.

An infant born to a 25-year-old gravida 2 para 1 mother by cesarean section at 36 weeks' gestation had loops of small intestine protruding from the abdominal cavity.

The parents of a 3-month-old infant sought medical advice because of a mass in the child's umbilical area. The mass increased in size when the infant cried, coughed, or strained and was reducible inside the abdomen by external pressure.

A 6-year-old boy presented with a mass on the left side of the scrotum. The mass did not vary in size and was asymptomatic; it transilluminated brightly. Physical examination showed it to be 4 × 2 cm. The spermatic cord could be felt above the mass. The left testis was impalpable separately.

The mother of a 2-year-old boy was concerned because his scrotum appeared flat and empty. (She had noticed this earlier but thought it was normal for her child's age.) On examination, the testicles were not palpable in the scrotum. They were found in the inguinal area and could not be manipulated into the scrotum. Bilateral orchidopexy was performed, and the postoperative course was uneventful.
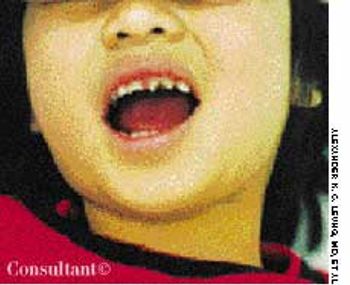
These notched upper central incisors were noted in a 3-year-old girl. There was no history of traumatic injury to her mouth. The youngster was able to sweat normally, and no other evidence of ectodermal dysplasia was present.

The parents of a 2-year-old boy were curious about the “bump” near their son's eye, which they had first noticed about 6 months earlier. The cystic mass in the right medial canthal region measured 8 mm in diameter. It was nontender.

The extent of mucosal or transmural intestinal necrosis varies. Pneumatosis progresses from the submucosa through the muscular layer to the subserosa. The distal ileum and proximal colon are most frequently involved.

Mongolian spots are congenital, hyperpigmented, usually gray areas of varying size and shape. They result from the abnormal occurrence of melanocytes in the lower half of the dermis and are found most frequently in the sacrococcygeal and gluteal areas.

These collections of dilated vessels deep in the dermis and subcutaneous tissue are present at birth. They usually present as bluish or reddish lesions that are cystic, firm, and compressible. About 60% to 80% of cavernous hemangiomas undergo spontaneous involution, often with central clearing and fibrosis.

Inspissated, sticky, immobile meconium causes this transient form of distal colonic or rectal obstruction in newborns. The incidence has been estimated at 1 in 500 to 1000 live births. The condition is thought to result from dehydration of the meconium.

These are hyperpigmented, regularly bordered, sharply demarcated macules that are usually tan or light brown in whites and dark brown in dark-skinned persons. The lesions are characterized by an increased number of melanocytes and an increased amount of melanin in the epidermis.

This newborn has Cornelia de Lange syndrome, a disorder characterized by prenatal growth retardation (this child weighed 2240 g at birth and measured 46 cm in length), microbrachycephaly, bushy eyebrows, long eyelashes, short neck, low posterior hair line, depressed nasal bridge, anteverted nares, long philtrum, thin upper lip, downturned corners of mouth, micrognathia, a single umbilical artery, phocomelia, micromelia, and oligodactyly.

This newborn has trisomy 18, as manifested by intrauterine growth retardation (birth weight, 2350 g; length, 47.2 cm), microcephaly (head circumference, 31.5 cm), short neck, hypotonia, feeding difficulties, high-pitched cry, micrognathia, cleft palate, low-set ears, short sternum, widely spaced nipples, clenched hands with ulnar deviation and overlapping digits, micromelia, and a single umbilical artery.
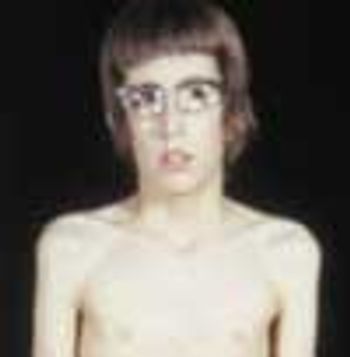
The parents of a 10-year-old boy of normal intelligence brought him for evaluation because of his tall stature. He was 154 cm tall (3 cm above 97th percentile) and weighed 34.3 kg (50th percentile). He exhibited significant arachnodactyly, with an upper to lower segment ratio of 0.8 and an arm span to height ratio of 1.1. He had a long, angular face with a high arched palate and crowded dentition, ptosis, myopia, superior lens subluxation, pectus excavatum, widely spaced and low-set nipples, grade 2/6 ejection systolic murmur at the left sternal border, midthoracic scoliosis, joint hypermobility, positive thumb sign and wrist sign, and pes planus.

This 8-year-old girl was born with multiple congenital anomalies. The child had broad, short feet; postaxial polydactyly of the feet bilaterally; brachydactyly of the hands; cystic dysplasia of the kidneys; a single atrium; ventricular septal defect; retinitis pigmentosa; flat nasal bridge; and anteverted nares.

The nonpruritic hypopigmented lesions on this 13-year-old girl's cheeks are characteristic of pityriasis alba, which typically occurs in children of both sexes between the ages of 3 and 16 years.

A mass on the left side of the scrotum was the presenting complaint of a 7-year-old boy. The mass increased in size when the child cried, strained or coughed. Physical examination showed a left scrotal mass that was reducible with manipulation when the child was lying down. The left spermatic cord was found to be thickened-the "silk" sign.

Two weeks after the subcutaneous injection of 0.5 mL of varicella vaccine in a 2-year-old girl's left arm, a nonpruritic rash developed on the child's upper abdomen and left forearm. She had no fever. The lesions subsided after 5 days.

This 7-month-old infant had light red macules on the glabella that were first noted at birth. By the time the child was 2 years old, the lesions were only faintly visible.

An 18-month-old girl was noted to have somatic overgrowth, macroglossia, macrostomia, fading telangiectatic nevi over the glabella and eyelids, vertical creases on the earlobes, a short nose with anteverted nares, and a long philtrum. She also had an ejection systolic murmur best heard at the left mid- and upper sternal border, compatible with an atrial septal defect.