
The lesion’s location, along with visible telangiectasia on the lesion’s surface, suggest a basal cell carcinoma.

The lesion’s location, along with visible telangiectasia on the lesion’s surface, suggest a basal cell carcinoma.

Note that some lesions occur within the outer ear, quite typical for the diagnosis of discoid lupus.

Up to 80% of those with necrobiosis lipoidica have diabetes mellitus; however, this disorder develops in fewer than 1% of people who have diabetes.

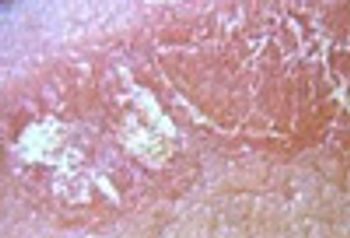
This solitary, fairly well-defined whitish plaque, surrounded by a broad band of violaceous erythema is a classic presentation of the “lilac ring” phase of early morphea. Potent corticosteroids led to prompt resolution.

The differential diagnosis includes figurate erythema, granuloma annulare, sarcoidosis, and Hansen’s disease. Additional history disclosed that the plaques expanded, migrated and disappeared over a matter of days, eliminating all but the correct diagnosis: figurate erythema, a reactional (hypersensitivity) state.

The location (pretibial surface) of this ulcer, its visibly rolled undermined border, and severe pain are all typical of pyoderma gangrenosum, which is typically associated with inflammatory bowel disease, rheumatoid arthritis, and hematologic malignancies.

This is the most common form of amyloid deposition in the skin. It is not associated with the systemic disease, but is solely a cutaneous malady.

These whitish colored lesions were the result of lichen planus. Hepatitis C virus infection should be sought, since this viral infection is often associated with recent-onset lichen planus in younger persons.

In older persons, tense blisters such as these are most likely bullous pemphigus, an autoimmune blistering disease. Biopsy as well as direct and indirect immunofluorescent tests may be needed to exclude other blistering diseases, such as pemphigus and epidermolysis bullosa.

This is classic vitiligo, an autoimmune disease in which anti-melanocyte antibodies develop. Phototherapy or topical calcineurin inhibitors may be beneficial.
The fairly well-defined erythematous plaques covered with silvery scale are typical for psoriasis. In some patients, the disorder may be limited to the genital skin.

The patient knew that he had psoriasis, but failed to connect onychodystrophy to his underlying skin disease.

A biopsy confirmed that the white mucosal discoloration and scattered small erosions were the result of lichen planus. Eradication may be attempted with potent topical steroids or oral steroids.

This man wore a personal heart rate monitor/transmitter while running, and had become allergic to the thiuram chemicals used to make the synthetic elastic band. A topical corticosteroid resolved the problem.

Bruising is a sign/symptom to be taken seriously. This patient abused alcohol; his vitamin C deficiency confirmed the diagnosis of scurvy. This patient is also at risk for pellagra and beri beri.

Despite the fact that this lesion is NOT in a sun-exposed skin site, the clinical features are typical for a basal cell carcinoma.

Pitted keratolysis is caused by pedal hyperhidrosis and subsequent overgrowth of bacteria that produce proteinases that dissolve keratin and lead to pit formation.

Most bruising episodes are directly related to trauma, medication, or herbal supplements. When no no clear etiology is prsent, "spontaneous" bruising should be considered an urgent problem.

Each of these lesions proved to be infiltrative basal cell carcinomas. Denial is a strong defense mechanism and it can lead patients to avoid seeking medical attention for long periods, as was the case here.

A small punch biopsy showed basal cell carcinoma with focal hypermelanosis. The underlying erythema and punctuate superficial dark black pigmentation strongly suggested a dysplastic nevus or even a melanoma.

This was presumed to be an ectoparasite bite when the patient reported that she had a new pet kitten. A myriad of diagnostic possibilities exist, including the start of a drug eruption or viral infection, early allergic contact dermatitis, or first manifestation of an autoimmune bullous disease.
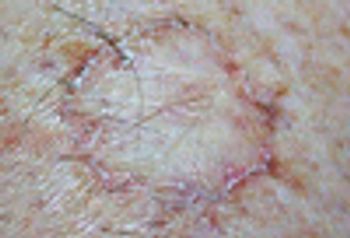
These hypopigmented well demarcated round patches with an atropic center are typical of porokeratosis, which can appear at any age.

The easily visible 5 mm-long insect, is a classic bedbug (Cimex lectularis).

A biopsy is the only way to determine if this is a primary cutaneous neoplasm or a cutaneous metastasis from a visceral carcinoma.

This woman is allergic to an ingredient in her favorite lipstick.

A biopsy is mandatory since the diagnosis includes melanoma. This blue-black macule proved to be a blue nevus.

Mammography showed a dense fine mass which, on fine needle aspiration, showed intraductal carcinoma.

A painful and/or tender subungual lesion should suggest a “glomus tumor”-- a benign growth seen more commonly in women than in men and most frequently under the fingernail.

A number of clues suggest that this pigmented lesion is a seborrheic keratosis, including its rough surface, truncal location, and age of the patient (59 years).

Leishmaniasis remains an important infection which can be “imported” from endemic foci, such as the Middle East.