
Here we provide a list of questions with links that can help you respond to patients who may be asking you about H1N1 virus infection (swine flu). Topics include travel restrictions and recommendations for persons with chronic disorders.

Here we provide a list of questions with links that can help you respond to patients who may be asking you about H1N1 virus infection (swine flu). Topics include travel restrictions and recommendations for persons with chronic disorders.

A 50-year-old woman presents to the emergency department with severe dizziness, weakness, and dyspnea of 1 week’s duration. Ten days earlier, an upper respiratory tract infection (URTI) was diagnosed; over-the-counter cough syrup and acetaminophen were prescribed. However, the patient’s condition has steadily deteriorated since then. In addition, her urine has darkened over the past few days.

A 24-year-old man presented to the emergency department with worsening dyspnea and fever of 1 day’s duration. About 3 years earlier, he had been treated for testicular cancer (leiomyosarcoma) with orchidectomy, chemotherapy, and radiation. He had no significant social or family history. Temperature was 38.6°C (101.4°F); blood pressure, 119/80 mm Hg; heart rate, 121 beats per minute; and respiration rate, 20 breaths per minute. Oxygen saturation measured with pulse oximetry was 98% with a nonrebreather mask and about 80% without a nonrebreather mask. Breath sounds were decreased bilaterally. The abdomen was soft. Extremities were nonedematous. Neurological findings were intact with no focal deficits.

During the evaluation of a 61-year-old man who had sustained mild head and upper trunk injuries in a car accident, a right lower lobe consolidation was noted on the chest radiograph. There was no evidence of rib fracture. A chest CT scan with contrast showed a hilar mass that obstructed the lateral segmental bronchi of the right lower lobe. Atelectasis of the posteromedial segments of the right lower lobe and ipsilateral subcarinal adenopathy were also noted.

For 3 days, a 45-year-old woman with HIV infection who was noncompliant with her antiretroviral medications had cough, yellowish sputum, fever, and dyspnea. She denied hemoptysis, weight loss, or recent hospitalization. She had a long history of heavy smoking and alcohol and intravenous drug abuse.
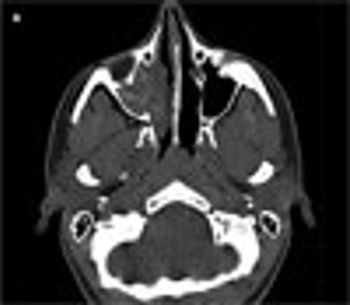
An 18-year-old woman with a history of allergic rhinitis and moderate persistent asthma presented with right-sided nasal congestion of 6 months’ duration. Her symptoms persisted despite her usual allergy medications, allergen immunotherapy, and 2 courses of antibiotics. A sinus CT scan showed complete opacification of the right maxillary sinus with increased attenuation of the mucin. Allergic fungal rhinosinusitis was suspected, and an otolaryngologist was contacted.

One way to determine whether a patient's asthma is well controlled is to inquire about the frequency of rescue treatments with an albuterol metered-dose inhaler.

Parents of young children know that colds are extremely common, especially from fall until spring. Colds account for a large number of pediatric office visits and telephone calls-particularly during "cold season."

New guidelines for community-acquired pneumonia (CAP) issued jointly by the Infectious Diseases Society of America and the American Thoracic Society emphasize the need for communities to adapt the recommendations to local conditions.

In the vast majority of nonsmokers who are not receiving angiotensin converting-enzyme inhibitors and who have no evidence of active disease on chest radiographs, chronic cough is caused by postnasal drip syndrome (recently renamed upper airway cough syndrome [UACS]), asthma, non-asthmatic eosinophilic bronchitis, or gastroesophageal reflux disease (GERD), alone or in combination.

Given the dramatic advances in antimicrobials since penicillin was introduced, why has the mortality rate associated with community-acquired pneumonia (CAP) remained essentially unchanged?

Take this MedPage Today poll on the accessibility of influenza vaccine.

MINNEAPOLIS -- Influenza vaccination reduces older adults' risk of hospitalization and mortality, researchers affirmed, despite lingering questions.

ROCKVILLE, Md. -- Afluria was approved today by the FDA as the sixth seasonal influenza vaccine on the U.S. market. Manufactured by Australia's CSL Limited, the company will produce about two million doses for this year's flu season.

WASHINGTON -- Influenza vaccination may save many fewer older patients' lives than generally claimed, according to researchers here.

ATLANTA -- Influenza vaccination rates have not rebounded after widespread vaccine shortages in the 2004-2005 flu season, CDC investigators said.

ROCKVILLE, Md. -- The FDA has expanded the indications for FluMist, a nasal influenza vaccine, to include children ages two to five.

abstract: While the risk factors for aspiration pneumonia are similar to those for aspiration pneumonitis, the 2 syndromes have different presentations. Aspiration pneumonia tends to occur in older patients or in those with neurological diseases, and the aspiration is not usually witnessed. Aspiration pneumonitis is more likely to occur in patients undergoing anesthesia or in those with acute drug and alcohol overdoses, and the aspiration is often witnessed. The workup may include bedside assessment of the cough and gag reflexes, chest radiography, videofluoroscopic imaging, or fiberoptic endoscopy. Empiric antibiotic therapy should be avoided in most patients with pneumonitis; however, antibiotics may be indicated for those at high risk for bacterial colonization of oropharyngeal and gastric contents who have fever, increasing sputum production, or new infiltrates or for those who fail to improve within 48 hours. (J Respir Dis. 2007;28(9):370-385)

A 43-year-old woman presented to the emergency department with complaints of severe dyspnea, wheezing, and cough productive of white sputum. She had received a diagnosis of asthma 3 years earlier, based on symptoms of wheezing and cough. Since then, her drug regimen has included intermittent use of albuterol.

Evaluation of a radiograph's quality requires some understanding of the technical factors involved in the production of an x-ray image. Without such understanding, the risk of making an interpretive error is increased.

A 52-year-old woman presented to her primary care physician complaining of a nonproductive cough and dyspnea on exertion. These symptoms had a subacute onset over 4 weeks before her initial visit. She denied fever, sputum production, hemoptysis, chest pain, palpitations, abdominal pain, nausea, vomiting, and diarrhea. She did not have any known sick contacts.

abstract: Common causes of poorly controlled asthma include nonadherence to long-term inhaler therapy; environmental exposures; and uncontrolled comorbidities, such as allergic rhinitis. Adherence can be limited by many factors, including inadequate patient education, medication cost, prior failed treatment, poor physician-patient relationship, unrealistic expectations for therapy, and depression. For patients who have a poor perception of their symptoms, emphasizing the "disconnect" between symptoms and pulmonary function can help motivate them to monitor themselves with a peak flow meter and to adjust their medication accordingly. For patients with allergic triggers, instituting allergen-specific environmental controls can decrease symptoms and urgent care visits for asthma. Chronic rhinosinusitis and gastroesophageal reflux disease can also contribute to difficult-to-control asthma, and treatment of these comorbidities can help reduce asthma symptoms. (J Respir Dis. 2007;28(9):365-369)

TUCSON, Ariz. -- For many adults with poor airway function or COPD, the genesis of the problem may have been in the womb, researchers reported.

ABERDEEN, Scotland -- COPD patients may be as much at risk from air pollution inside their homes as they are outside, researchers found.

COLUMBUS, Ohio -- Spirometry can help emergency departments distinguish between the wheezing of acute asthma in adolescents and vocal cord dysfunction, found investigators here.