
Findings from the ECLIPSE clinical trial showed the blood-based cancer screening test detects 83% of people with CRC, with a specificity of 90%.

Findings from the ECLIPSE clinical trial showed the blood-based cancer screening test detects 83% of people with CRC, with a specificity of 90%.
Over 4 million cancer deaths have been reverted since 1991, but new cancer cases are estimated to reach over 2 million, according to new data from an annual American Cancer Society report.

Data from recent Austrian study suggest that sex should be considered when determining screening age for colorectal cancer, reported authors.

Your daily dose of the clinical news you may have missed.

A pivotal phase 3 clinical trial showed Cologuard significantly more likely than FIT to detect cancerous and advanced precancerous lesions.
The American College of Physicians in the updated guidance maintains the risk/benefit ratio supports screening initiation at age 50 (vs 45) years.

A combination of outreach measures tailored to the needs of rural Midwest women increased recommended screenings by as much as 6-fold.

New research shows excessive alcohol use is strongly associated with an increased risk for colorectal cancer, regardless of genetic risk.

A new study found that women who consumed ≥2 servings/day of sugar-sweetened beverages had a 2.2-fold higher risk for early onset CRC vs those who had less than 1 serving/week.
For the first time, the USPSTF recommends colorectal cancer screening in adults beginning at age 45.

A large review ties nut consumption to a lower incidence of cancer, but not diabetes.

Is a surveillance interval of 1 year, 3 years, 5, or 10 years recommended?

Certain patients with inflammatory bowel disease are at heightened risk for the development of colorectal cancer. But researchers have not yet been able to discover markers that can identify these patients.

A 47-year-old woman who recently completed adjuvant chemotherapy for colon cancer has painless cervical lymphadenopathy of 1 to 2 cm. She has no fever, sore throat, cough, or unexplained weight loss, and she denies exposure to ill persons or animals.

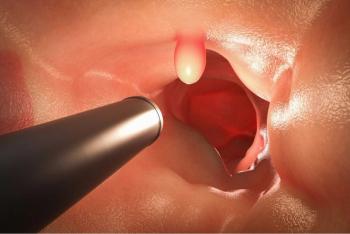
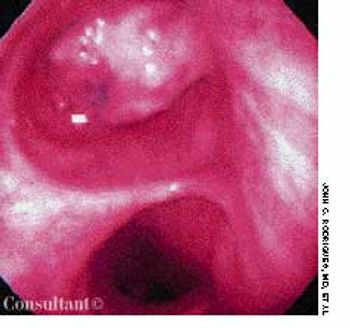
ABSTRACT: Screening options for colorectal cancer (CRC) include colonoscopy every 10 years, annual fecal occult blood testing, flexible sigmoidoscopy every 5 years, or double contrast barium enema every 5 years. In white patients at average risk, screening should begin at age 50; in African American patients, at age 45. Colonoscopy is preferred to sigmoidoscopy because it can detect proximal neoplasms and has the longest protection interval. High-risk patients include those with a family history of CRC or adenomas. These persons should begin colonoscopic screening at age 40, or 10 years earlier than the age at which CRC or adenomas were diagnosed in a first-degree relative. Other high-risk patients are those with a personal history of CRC, a genetic syndrome, or inflammatory bowel disease. In patients with CRC, the first follow-up colonoscopy is performed 1 year after surgery. If results are normal, the interval can be extended to every 3 years.

The FDA has approved injectable Acetadote (acetylcysteine)from Cumberland Pharmaceuticals Incto prevent or lessen liver damage resulting from an overdoseof acetaminophen. According to the FDA, unintentionalacetaminophen overdose is responsible for 100deaths and 56,000 emergency department visits per year.

As the population ages, physicians are seeing a greaternumber of patients with colorectal disorders. This book combinesan up-to-date survey of the latest basic and clinicalresearch in the field with practical advice for the day-to-daycare of patients with colonic diseases. The first section ofthe book covers current knowledge of normal colorectal physiology.Section 2 discusses the basic disease mechanismsinvolved in colonic disorders and reviews the uses of suchinvestigational tools as colonoscopy, colonic biopsy, anorectalmanometry, ultrasonography, motility measurement,defecography, CT, and MRI. The third section offers a fulldiscussion of the diagnosis and treatment of commoncolonic disorders, including colorectal neoplasia, inflammatorybowel disease, ulcerative colitis, diverticular disease,Crohn disease, constipation, and irritable bowel syndrome.In addition to currently recommended approaches to evaluationand treatment, chapters in this section include discussionof advanced and investigational therapies.

A 72-year-old man complains that he has been losing weightfor the last 2 months. Colon cancer was diagnosed 2 yearsearlier, and the lesion was resected; he did not receive anyadditional therapy at that time. Except for hypertension,which is well controlled with propranolol, the remainder ofthe medical history is unremarkable.

Highlights:➤What to tell your patients about thebenefits-and risks-of mammography.➤A realistic look at cancer screening: Arewe overstating the benefits?➤Which screening strategies you canrecommend with confidence.➤How best to bring the patient into thedecision-making process.

During a routine checkup, a middle-aged woman asks you whether she should stop wearing moisturizers and makeup that contain sunscreen. She has read that increased sunlight exposure enhances vitamin D production, which may prevent certain types of cancer. What would you tell her?

A 52-year-old woman was admitted tothe hospital with progressive shortnessof breath of 2 days’ duration. Bronchialasthma had been diagnosed 6 monthsearlier; inhaled corticosteroids, bronchodilators,and leukotriene antagonistswere prescribed. Despite aggressivetreatment, the patient’s dyspneaand wheezing worsened.

An 83-year-old man complains of weakness, easy fatigability, and poor appetitethat began 4 to 6 weeks ago. He becomes short of breath on his daily walksand has lost about 20 pounds over the last 3 months. He denies nocturia,paroxysmal nocturnal dyspnea, exertional chest pain, fever, cough, melena,and hematochezia. His only GI symptom is occasional crampy abdominal painwith bowel movements.

You routinely order laboratory screeningpanels, including serum liver enzymemeasurements, for nearly everypatient who has a complete physicalexamination or who is seen for any ofa host of other complaints. If you findabnormal liver enzyme levels, your familiaritywith the common causes andthe settings in which they occur mayenable you to avoid costly diagnosticstudies or biopsy.

An 80-year-old woman presented with recurrent abdominal pain for 1 month, constipation, and vomiting. She had no diarrhea, rectal bleeding, or weight loss.
Persistent collapse of the right lung led to hospitalization of a 62-year-old woman with a history of colon cancer. She had no fever, chills, rigor, or hemoptysis. The patient underwent bronchoscopy to rule out any central endobronchial obstructing lesion.