
Sudden profound vision loss in her left eye prompted an82-year-old woman to seek evaluation. She also complainedof ��“just not feeling well” and reported new-onsettemporal and occipital headaches of 6 weeks’ duration.

Sudden profound vision loss in her left eye prompted an82-year-old woman to seek evaluation. She also complainedof ��“just not feeling well” and reported new-onsettemporal and occipital headaches of 6 weeks’ duration.

A 49-year-old woman presented for aroutine eye examination. She had nohistory of systemic disease and tookno medications.

For 3 years, a linear plaque had been slowly developing on the left palm of a 47-year-old woman who had difficulty in opening and closing her hand. There was no contributory family history.

ABSTRACT: In high-risk patients with vascular disease, blockade of the renin- angiotensin system (RAS) can help prevent cardiac remodeling that ultimately results in left ventricular hypertrophy (LVH) and heart failure. Optimal treatment of these patients, who often have diabetes or renal disease, usually involves a combination of agents-1 of which should be a thiazide diuretic-to reduce blood pressure, control the comorbid condition, and prevent end-stage organ damage. The manner in which the RAS is interrupted may be important. For example, although a thiazide diuretic and an angiotensin-converting enzyme (ACE) inhibitor are recommended for hypertensive patients with LVH, an angiotensin II receptor blocker (ARB) in combination with a diuretic was recently found to reduce cardiovascular morbidity and mortality in these patients to a greater degree than a ß-blocker/diuretic. Both ACE inhibitors and ARBs delay the progression of diabetic nephropathy and reduce albuminuria. ARBs were recently shown to reduce progression from microalbuminuria to macroalbuminuria. In patients with systolic heart failure who cannot tolerate ACE inhibitors, an ARB can be used with a ß-blocker.

A 1-year history of “dents” on her body prompted a 40-year-old African American woman to seek medical evaluation. Her medical history was unremarkable; however, there was a strong family history of severe type 2 diabetes mellitus. The patient denied having received or having self-administered injections into the affected areas. She reported no history of deep, tender nodules at the sites.

A 62-year-old obese woman with adult-onset type 1 diabetes mellitus had a 6-year history of bilateral leg edema. During the last year, the edema worsened and the skin on her legs thickened. She also had multiple, bilateral, painful, superficial ulcers that drained copiously.

A 12-year-old African American girl comes to youroffice for a well-child checkup. She is tall for herage (height above the 95th percentile) and obese(body mass index [BMI] above the 95th percentile).Physical examination reveals acanthosisnigricans on her neck, axilla, and upper abdominalregion (Figure) and a vaginal yeast infection.Routine urinalysis reveals a glucose level ofgreater than 1000 mg/dL, with negative proteinand ketones. A random blood glucose test, obtainedbecause of the glucosuria, is 249 mg/dL.

ABSTRACT: Fibromyalgia syndrome (FMS) is a common condition that causes chronic pain and disability. It should be diagnosed by its own clinical characteristics of widespread musculoskeletal pain and multiple tender points. American College of Rheumatology criteria guidelines are most helpful in diagnosing FMS. The major symptoms are pain, stiffness, fatigue, poor sleep, and those of other associated conditions, for example, irritable bowel syndrome, headaches, restless legs syndrome, chronic fatigue syndrome, and depression. The pathophysiology of FMS is thought to involve central sensitization and neuroendocrine aberrations, triggered or aggravated by genetic predisposition; trauma; psychosocial distress; sleep deprivation; and peripheral nociception.

Foot ulcerations and infections are the leading cause of hospitalization amongpatients with diabetes; they occur in about 15% of these patients.

An obese 55-year-old woman had intermittent dysuria and frequent urination for 4 days and fever, abdominal pain, and vomiting for 3 days. Her history included type 1 diabetes mellitus, hypertension, and angina; her medications included insulin, nifedipine, and nitroglycerin.

A 59-year-old man, who was unable to walk, was brought to the emergency department with severe leg pain, worsening weakness, increasing fatigue, chills, and fever of 3 days' duration. The symptoms began after a round of golf. In addition to the leg pain, which particularly affected the calf muscles, the lower extremities were red and swollen.

Progressive abdominal distention, nausea, constipation, and mild abdominal pain developed in an 82-year-old woman 5 days after she underwent surgical repair of a left hip fracture. Her medical history was significant for Parkinson disease, type 2 diabetes mellitus, and hypertension.
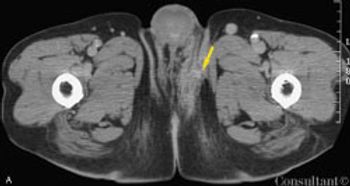
A 77-year-old African American man with type 2 diabetes mellitus and coronary artery disease presented to the emergency department with acute scrotal swelling and pain. His testicles were erythematous with focal areas of necrosis and associated tissue destruction. Similar skin changes were apparent in the lower abdominal and inguinal regions.

A 45-year-old woman presents with multiple injuries she sustained during a skiingaccident. She has fractures of her right arm and 3 ribs, as well as numerouscontusions. An abdominal CT scan shows no hemorrhage or other traumarelatedfindings; however, a 6.7-cm left adrenal mass is detected.

ABSTRACT: To identify the cause of hyponatremia, determine the patient's volume status and measure urinary sodium and osmolality; also ask about diuretic use. Hypovolemic hyponatremia is associated with vomiting, diarrhea, laxative abuse, renal disease, nasogastric suction, salt-wasting nephropathy, Addison disease, solute diuresis, and diuretic use. Euvolemic hyponatremia with a normal urinary sodium level can result from glucocorticoid deficiency, hypothyroidism, certain drugs, and the syndrome of inappropriate antidiuretic hormone secretion. Euvolemic hyponatremia with low urinary osmolality can be caused by psychogenic polydipsia, "tea and toast" syndrome, or beer potomania. Hypervolemic hyponatremia is associated with congestive heart failure, nephrotic syndrome, and cirrhosis. To reduce the risk of serious neurologic sequelae, avoid both undertreatment and overtreatment of hyponatremia. In chronic hyponatremia, total correction should not exceed 8 to 12 mEq/L/24 h (a maximum correction rate of 0.5 mEq/L/h). In acute hyponatremia, rates of correction up to approximately 1 mEq/L/h are acceptable. Avoid overcorrection of serum sodium concentration (ie, to a level higher than 140 to 145 mEq/L).

A blue-black nodule has been present next to a 19-year-old woman’s left eyesince birth. After recent accidental trauma, the lesion has enlarged.

A 75-year-old man was brought to the emergency department with fever, cough, and abdominal pain of 2 days’ duration. The pain was most severe in the epigastric and umbilical regions. The patient’s history included type 2 diabetes mellitus, hypertension, and hypercholesterolemia. He had smoked cigarettes for 40 years and recently lost 50 lb. The patient was tachypneic and diaphoretic.

A network of purplish pink lesions recently developed on a 28-year-old woman’sarms and legs. The asymptomatic rash becomes more prominent with exposureto cold. The patient denies fever, aches, arthralgias, oral erosions, chestpain, and photosensitivity.

Three weeks after coronary artery bypass graft (CABG)surgery, a 52-year-old woman complained of pain at thesternal scar. The patient had a history of diabetes and hypertension.She had smoked cigarettes for many years.

Three weeks after coronary artery bypass graft (CABG)surgery, a 52-year-old woman complained of pain at thesternal scar. The patient had a history of diabetes and hypertension.She had smoked cigarettes for many years.

A 54-year-old man is admitted to the hospital because of worsening lower extremityswelling and knee and ankle pain and stiffness. These symptoms havemade walking very difficult for the past month.

For 2 months, a 47-year-old woman experienced constipation, weakness, fatigue, and dry skin. She also complained of moderate weight gain and menorrhagia during the same period. The patient took no medications and denied any allergies.

A 42-year-old woman complains of anxiety, unexplained weight loss, and palpitationsthat started about 3 weeks earlier. She denies fever, trauma, and newstress. She has a history of several urinary tract infections for which imagingfailed to reveal any predisposing factors; all were successfully treated withmedication. The remainder of the history is unremarkable.

A 78-year-old man presented to theemergency department with a 3-weekhistory of progressive shortness of breathand cough with blood-streaked, yellowishsputum. The patient had dyspnea onexertion limited to 2 blocks, 2-pilloworthopnea, paroxysmal nocturnal dyspnea,and nocturia. Neither fever norchills were present. He had lost 7.2 kg(16 lb) during the last year.

A 44-year-old man with type 2 diabetes was recently hospitalized for an acuteexacerbation of pancreatitis. This was his seventh admission for the conditionwithin the past several years. Although imaging studies revealed no calcifications,the hospitalist suspected that acute relapsing pancreatitis was evolvinginto chronic pancreatitis.