
Here: 10 tips that can help you provide optimal care of your patients with MS.

Here: 10 tips that can help you provide optimal care of your patients with MS.



In many patients, episodic migraines increase in frequency and transform into a refractory pattern.

What are the factors that underlie the transformation of episodic migraine to refractory migraine? Dr Susan Hutchinson explains.

A bad ("sick" or killer) headache is usually a migraine if underlying organic causes of pain are ruled out.

When counting sheep fails as first line therapy, what measures can you recommend to help your patient get some sleep?

In Part 2 of this podcast series, Dr Smith continues his discussion of the practice of nonsuicidal self-injury in adolescents.

Early differentiation of epileptic from nonepileptic seizures is important. Clues that suggest epilepsy are a history of febrile seizures (particularly if prolonged), past brain injury from trauma or infection, and epilepsy in first-degree relatives.

In this podcast, Dr Smith discusses the practice of nonsuicidal self-injury in adolescents-cutting, burning, self-hitting or banging, scratching, interfering with wound healing-may be increasing.
A 59-year-old woman had aphasia and right-sided weakness after a routine total knee replacement. CT and MRI scans revealed a large left middle cerebral artery infarct. A CT angiogram showed no significant disease of the cerebrovascular arteries. Test results for the lupus anticoagulant were positive. A venous study of the legs showed no deep venous thrombosis. She was treated with warfarin and aspirin and discharged. After speech and physical therapy, she had mild residual aphasia.

Psychiatrist Sidney Zisook, MD-a guest speaker at the recent American College of Physicians meeting in San Diego

Warm weather can impair the ability of persons with multiple sclerosis (MS) to learn, remember, and process information, according to research presented at the American Academy of Neurology’s 63rd Annual Meeting in Honolulu April 9 to April 16, 2011

Multiple sclerosis (MS) is less likely to develop in persons with high levels of sun exposure and vitamin D, reported Australian researchers in the journal Neurology. This finding confirms the results of previous studies that showed MS occurs more frequently at latitudes farther from the equator

Cannabis worsens cognitive function in patients with multiple sclerosis, reported investigators recently in the journal Neurology. Marijuana has been used to relieve the pain and spasticity associated with MS; however, the results of this study show that the drawbacks may outweigh the purported benefits

The treatment of chronic fatigue syndrome (CFS) is mainly supportive. The key to effective management is to establish a therapeutic alliance with patients and to convey a consistent message that their complaints are taken seriously. Although spontaneous recovery is rare, it does occur in some patients with CFS.

Chronic fatigue syndrome (CFS) is a distinct disorder characterized by debilitating and often recurrent fatigue that lasts at least 6 months but more frequently lasts for longer periods. Patients with CFS experience overall physical, social, and mental impairments and may subsequently qualify for medical disability.

Primary care is demanding for a host of reasons, not the least of which is the daunting breadth of issues practitioners grapple with. One issue is evaluating the risk of suicide. Two recent studies provide some intriguing data that may change the way we practice.

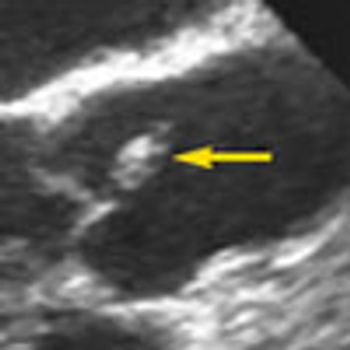
For the past year, a 52-year-old man had dysphagia, which he described as a “knot stuck in the throat” and an associated 25-lb weight loss. He denied fever, chills, headache, abdominal pain, and diarrhea. The patient had been living in the Dominican Republic until about 1 year earlier, when he moved to the United States. He had a 30 pack-year smoking history; he also had hypertension, asthma, and coronary artery disease (none of which were pharmacologically treated). He denied alcohol and illicit drug use.
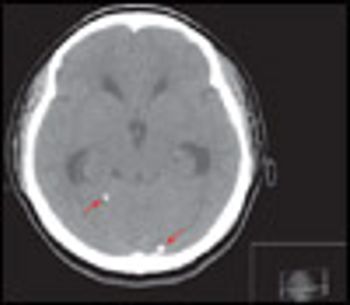
An 18-year-old woman from Mexico was hospitalized because of severe headache with nausea and vomiting. Her headaches had started 4 years earlier and had progressively worsened. They occurred mainly in the occipital region and were pulsating, worse on bending down, and unrelieved by any medication. They were often accompanied by dizziness and presyncope.

After listening to the previous 3 podcasts, you may be wondering how to begin a therapeutically valuable conversation with your patient, which will provide the critical details that you need in the short time that you have. In his final podcast, Dr Lieberman offers a list of questions that you can use to break the ice and kick start a dialog with a patient whom you suspect has a mental health disorder.

It can sometimes be difficult to detect the fine tremors of the hands and fingers of a patient with hyperthyroidism.

A 65-year-old man, who was lost to follow-up after abdominal-perineal resection for rectal adenocarcinoma 9 months earlier, presents with progressively worsening neurological symptoms, including bilateral hearing loss, dizziness, gait disturbance, ataxia, and blindness in the right eye.
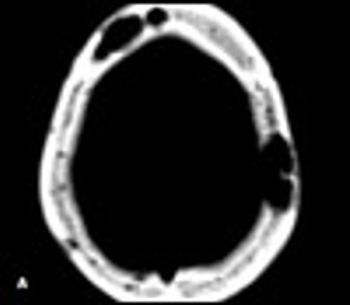
A39-year-old man with a history of AIDS and nonadherence to highly active antiretroviral therapy (HAART) presented with frontal headache and scalp pain of 2 weeks' duration. These symptoms were accompanied by nausea, weight loss, and generalized weakness. Physical examination revealed a small, tender scalp lump, 2 × 2 cm over the left parietal area. The findings from the rest of the examination were unremarkable.

Primary care physicians treat the majority of patients in this country who have mental health disorders. But how well prepared are we for these patients when they present to our offices?