
LOS ANGELES ? Children with headaches are more likely to be overweight or obese, researchers said here.

LOS ANGELES ? Children with headaches are more likely to be overweight or obese, researchers said here.

A 15-year-old boy complains of moderate to severe headaches that occur daily and usually last all day; the pain typically worsens toward the end of the day. How will you help this patient?

Which test--antistreptolysin O titers, coronary angiography, enzyme-linked immunosorbent assay (ELISA), Western blot testing for Borrelia burgdorferi, or genetic testing for long QT syndrome--would help you diagnose a young man with worsening chest pain, frontal headache, and diffuse muscle and joint pain?

A 79-year-old woman with a 37-year history of type 2 diabetes mellitus complains of head pain that began more thana month ago and is localized to the left frontotemporal region. She characterizes the pain as constant and burning, with minimalfluctuations in intensity. The pain does not increase with any particular activity but is quite disabling; it has causedemotional lability and insomnia. She denies nausea, visual disturbances, weakness of the extremities, dizziness, or tinnitus.Her appetite is depressed; she has experienced some weight loss.

Delirium in older adults needs to berecognized early and managed as amedical emergency. Prompt detectionand treatment improve both shortandlong-term outcomes.1,2 Becausedelirium represents one of the nonspecificpresentations of illness in elderlypatients, the disorder can be easilyoverlooked or misdiagnosed. Misdiagnosismay occur in up to 80% of cases,but it is less likely with an interdisciplinaryapproach that includes inputfrom physicians, nurses, and familymembers.3

A 28-year-old man presented with chest pain, hemoptysis, and wheezing. He had a history of intermittent shortness of breath that occurred at least 3 times a year in the past 3 years; fever; and loss of appetite associated with headache, vomiting, and weakness. His medical history also included asthma, chronic gastritis, and more than 5 episodes of pneumonia since 1996. A test for hepatitis C virus (HCV) had yielded positive results.

The patient presented with left-sided, throbbing headaches that had gradually increased in severity and frequency. These headaches, which occurred once or twice a month, were associated with photophobia, phonophobia, and nausea, and usually lasted 8 to 12 hours. The headaches affected the patient's job performance and attendance, and she complained of fatigue, lack of sleep, and difficulty in concentrating.

A 36-year-old man with a 15-year history of episodic migraine presents to the emergency department (ED) at 5 AM witha right-sided throbbing headache of 4 hours' duration. The headache awakened him, which is typical of his more severemigraine attacks. Unfortunately, the patient forgot to refill his prescription for pain medication and did not "catch" thisheadache in time. He took an over-the-counter combination of aspirin and caffeine, which seemed to help for about 60minutes, but the headache has returned full force. He has vomited twice-another characteristic typical of his migraineattacks

I suspect that my patient has hereditary angioedema (HAE). During her lastpregnancy 2 years earlier, she had severe preeclampsia.

This is a difficult question, because most "sinus headaches" are migraines.1-3 In fact, there is no such thing as a sinus headache. The International Headache Society (IHS) defines a headache attributable to rhinosinusitis according to the criteria listed in Table 1.4 This requires a diagnosis of acute rhinosinusitis and a headache that occurs at the same time.

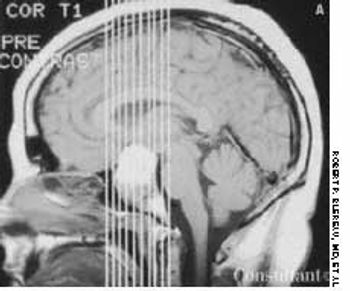
Chronic headache that worsened when she bent forward and episodes of usually unilateral vision loss sent a 34-year-old woman for medical consultation. The vision loss occasionally occurred in both eyes simultaneously.

What are the current recommendations for hormonal contraception (eg, oralcontraceptives, medroxyprogesterone injections) in patients with migraine?

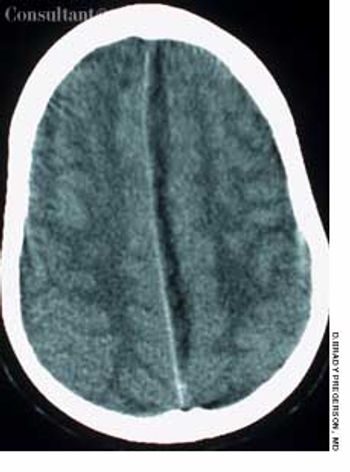
As many as 300,000 sportsrelatedconcussions arediagnosed each year inthe United States.1 Thisfigure underestimatesthe true incidence, however, becausemany concussive injuries are notrecognized by the injured persons,trainers, or physicians. A recentstudy found that 4 of 5 professionalfootball players with concussionwere unaware that they had sufferedthis injury.2

A neurologic deficit caused by a transient ischemic attack should last less than 24 hours. This woman presented with signs of paresis that had persisted for 36 hours, thus ruling out transient ischemic attack.

A 71-year-old man presented with a 6-week history of decreased vision in his right eye. The patient, who had hypertension and migraine headaches, had successfully recovered from a stroke that occurred 1 year earlier. His medications included aspirin, 81 mg/d, clopidogrel, atenolol, and furosemide. He also took gabapentin, 300 mg hs, for his migraine headaches. He had a remote history of cigarette smoking.

What are the current recommendations for the use of corticosteroids in the treatment of migraine? Is this a therapy primary care clinicians might consider?

A 51-year-old man with a history of AIDS (CD4 count of 59 cells/µL), anemia, neutropenia, and AIDS-related dementia presented with persistent fever, abdominal pain, and diarrhea of 2 months' duration. He did not adhere to his regimen of HAART and prophylactic therapy with atovaquone and azithromycin.

A 45-year-old man presented to the emergency department (ED) with fever and left-sided pleuritic chest pain. He had been in good health until 4 days earlier, when diffuse myalgias, weakness, and frontal headache developed. Two days later, these symptoms were accompanied by onset of fever (temperature, 39.4°C [103°F]) and left-sided pleuritic chest pain. He denied chills, rigors, shortness of breath, hemoptysis, and cough.

A 24-year-old woman complains of a severe, throbbing headache that is present when she is upright and is relieved when she lies down. When she is upright, she also experiences dizziness, blurred vision, light sensitivity, nausea, and occasional diplopia.

A physician who has chronic daily headaches is concerned that his alprazolam regimen (0.5 mg of alprazolam nightly) may be considered "excessive use."
After being hit on the head during a football game, a 16-year-old experienced several seconds of complete vision loss in the left eye. A few days later, he noticed the onset of blurred vision in the same eye, which progressively worsened over several weeks.
A 74-year-old man, who had been aware of a gradual increase in hat size over the past 3 years, complained of a mild headache and backache. His serum phosphatase level was 1,475 U/L (upper normal limit, 120 U/L). Skull films showed calvarial enlargement caused by thickening of the cortical tables, radiolucency in the frontal and occipital regions, and patchy osteosclerosis that produced a cotton-wool appearance.
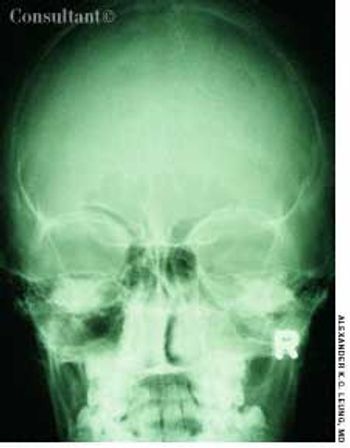
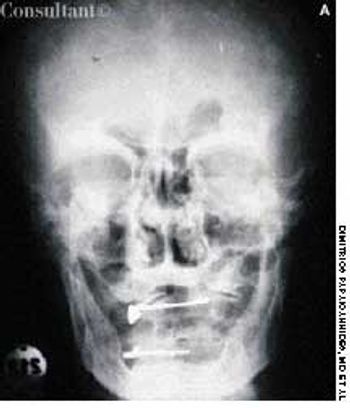
A 10-year-old boy had a headache, fever, cough, and nasal discharge for 2 days. His temperature was 38°C (100.4°F). Mucopurulent, yellow nasal discharge, fetid breath, and tenderness over the maxillary area were noted.
For 7 days, a 10-year-old boy had had a headache and a fever (temperature, 38.8°C [102°F]); a viral upper respiratory tract infection had been diagnosed. His parents brought him to the emergency department when weakness in his right leg developed, which impaired walking.

A 6-year-old girl was evaluated in the emergency department for a leg rash that had spread to the buttocks. The lesions first appeared earlier in the day and worsened hourly. The child's mother reported that her daughter was in good health until a low-grade fever, nonproductive cough, sore throat, and headache developed 5 days earlier. The youngster also complained of neck pain with movement.