
The patient had been having slurred speech and trouble swallowing and chewing. He had been using his hand to hold his jaw closed and to push his jaw up to help him chew.

The patient had been having slurred speech and trouble swallowing and chewing. He had been using his hand to hold his jaw closed and to push his jaw up to help him chew.

Here: more evidence that with the proper tools and motivation, health and wellness are attainable goals-even within the constraints of MS.

Here, Armistead Williams, III, MD, of the International Multiple Sclerosis Management Practice in Manhattan, speaks directly to neurologists about the hard questions that need to be addressed about this complex illness.

What is a safe, effective, and inexpensive way to reduce the risk of heart attacks, strokes, and dementia? What we eat is a key part of the answer. For one thing, doctors can suggest an appropriate diet to motivated patients, or to those who prefer a non-drug approach.

School performance is more likely to be below average in children who have migraine than in those who do not have headaches.

Here: a project that sheds some light on the potential of an integrated and holistic approach to therapy for patients with multiple sclerosis.

What happens when complementary and alternative therapies are combined with traditional treatments in patients with multiple sclerosis? A new study suggests some positive benefits. Details here.

Venous thromboembolism is twice as likely to develop in patients with multiple sclerosis than in controls. Although the absolute risk of VTE is low in MS patients, thromboprophylaxis may need to be considered.

Physical inactivity is more common among patients with multiple sclerosis (MS) than the general public-even though studies have shown that exercise can reduce the frequency and intensity of MS symptoms. Here's a motivational technique that may help.

Meta-analyses of all available data have shown that smoking is associated with a 50% increased risk of MS.

Low bone mass may manifest early in MS: this finding calls for an active approach to optimize bone health.

October 11th is National Depression Screening Day. But how do you screen, diagnose, and treat effectively given the time constraints of busy office practice?

Patients with multiple sclerosis are more than twice as likely to report migraines as controls, according to a recent meta-analysis.

Population-based studies have firmly established that relatives of patients with MS are at increased risk for the disease.

A recent meta-analysis of all published studies showed that women with MS who decide to breast feed are almost half as likely to experience a postpartum relapse compared with women who do not.

Although genetics risk explains the familial clustering of MS, it cannot fully explain the geographic distribution of MS and the changes in risk that occur with migration. Infections have been suggested as a possible explanation. The most convincing candidate for involvement in MS is the Epstein-Barr virus.

Here: evidence that disease-modifying therapies can positively affect the long-term evolution of multiple sclerosis.

Even at disease onset, patients with MS have significantly lower bone mineral density than healthy controls. Close attention needs to be paid to the bone health of these patients.

Evidence for a treatment effect of vitamin D in modifying the course of MS is less compelling than evidence of a preventive effect.

Physical therapy can specifically address mobility deficits associated with multiple sclerosis-if the patient is referred early on in the disease’s course.

How to assess the degree of cognitive impairment in your MS patient if you work outside of a major medical center and have little access to experts trained to administer cognitive tests? BICAMS can help. Details from an expert here.
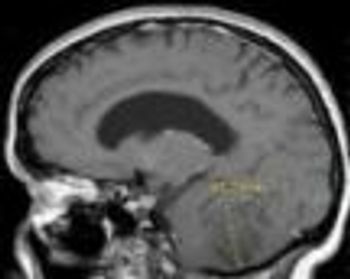
Lhermitte-Duclos disease is a rare, slow-growing, benign lesion of the cerebellum and is considered a hamartomatous tumor of the cerebellar cortex.

Common MS exacerbation triggers: infection, vaccination, stress, smoking, vitamin deficiency, or environmental changes.

Vertebral artery dissection may be misdiagnosed as post-concussive syndrome, stroke, or TIA, based on neurologic symptoms. Always consider after neck trauma.

Use of aspirin in primary prevention of cardiovascular disease must be based on individual risk-benefit analysis and is not appropriate for patients at low risk.