
A 45-year-old man complained of blood in his urine. The patient had a 7-year history of chronic renal failure secondary to hypertension; he had undergone hemodialysis for the past 5 years.


A 45-year-old man complained of blood in his urine. The patient had a 7-year history of chronic renal failure secondary to hypertension; he had undergone hemodialysis for the past 5 years.
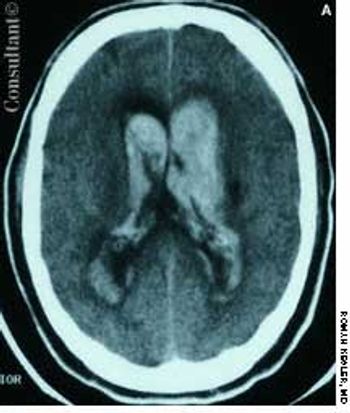
A 57-year-old man complained of a severe headache of sudden onset while he was lifting heavy boxes. Within minutes, he collapsed and became unconscious. On arrival at the emergency department, the patient was deeply comatose. His pupils were 7 mm, fixed, and unreactive to light; brainstem reflexes were absent, and he was unresponsive to noxious stimulation. His blood pressure was 210/120 mm Hg; he had no known history of hypertension.
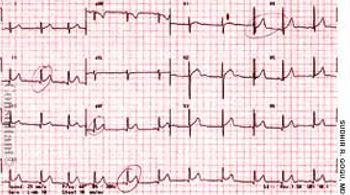
A 63-year-old African American man presented with orthopnea and pedal edema that had worsened during the past 4 months. Macroglossia was noted.
The mother of an 8-year-old girl sought medical care for her daughter who had complained of intermittent chest pain for 3 days. The patient denied nausea, vomiting, and diarrhea. There was no shortness of breath, chills, fever, or diaphoresis. Her travel history included 2 trips to Mexico within the past year; the most recent trip ended 3 months before the pain started.

A 48-year-old man complained of difficulty in swallowing both solid food and liquids. The dysphagia began several years earlier and had become increasingly severe and more frequent over the past 2 to 3 years. Vague heartburn without reflux and frequent regurgitation were also troublesome.
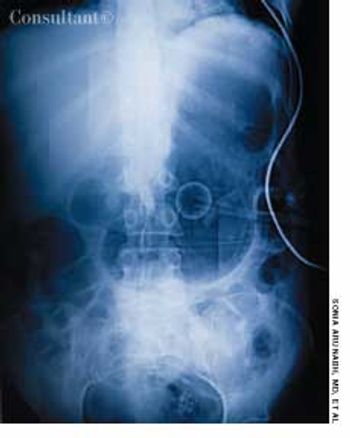
A 70-year-old man was brought from a nursing home to the emergency department with abdominal distention and vomiting of recent onset and a 2-day history of fever and abdominal pain. The patient had chronic obstructive pulmonary disease, type 2 diabetes mellitus, and hypertension. His gastric feeding tube, which had been placed via percutaneous endoscopic gastrostomy, was blocked.

A 75-year-old woman with a bioprosthetic aortic valve, who had undergone surgical repair of an aortic root aneurysm 9 months earlier was hospitalized with fever, headache, and altered mental status of 1-day's duration.

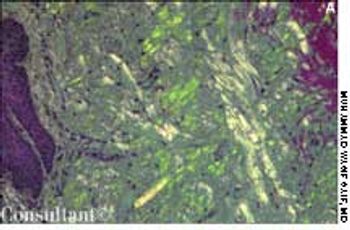
Systemic lupus erythematosus (SLE) was diagnosed in an 18-year-old man who presented with polyarthritis, fever, hypoxia, fatigue, anemia, neutropenia, and abnormal urinary sediment. A renal biopsy showed diffuse mesangial proliferative glomerulonephritis (World Health Organization class II). Serologic tests were positive for fluorescent antinuclear antibody (FANA), SS-A, SS-B, anti-Sm and anti-dsDNA antibodies, and rheumatoid factor; a direct Coombs' test result was positive as well.

Here are two cases that demonstrate the discovery of aortic aneurysms through careful and complete physical examination and via radiographic studies obtained to evaluate other conditions.
A 67-year-old woman presented to the emergency department (ED) with severe, sharp, central chest pain of sudden onset and mild shortness of breath. The pain had been present for 15 minutes. The patient was obese; her medical history included hypertension, myocardial infarction, and osteoarthritis.

A 54-year-old woman with a history of hypertension presented with a worsening headache and a left hemisensory defect. A CT scan of her head without contrast showed a right parietal hemorrhage with spreading edema; the masslike effect caused shifting of the midline to the contralateral side. The patient gradually became comatose and required intubation for airway protection. Intravenous corticosteroids were administered to decrease the effect of the lobar hemorrhage. Fever developed 3 days after admission.

Inflammation plays a major role in coronary artery disease (CAD), whereby inflammatory changes develop in the blood vessel walls.1 This observation has spurred interest in exploring the connection between CAD and markers of inflammation, including C-reactive protein (CRP), fibrinogen, serum amyloid A, and many other novel markers.

A 51-year-old man with a history of type B aortic dissection presented with severe right upper quadrant pain. He was febrile and hypotensive.

How much fish oil should I recommend that my patients with heart disease take?

Cardiovascular disease is a leading cause of death in patients with chronic obstructive pulmonary disease (COPD). While some physicians may be reluctant to prescribe ß-blockers for these patients, because of concern about adverse effects on lung function, a study conducted by Au and associates indicates that ß-blockers may have an edge over other antihypertensive agents in reducing mortality risk.

For 2 years, a 79-year-old man had postprandial fullness and epigastric discomfort. He also experienced regurgitation and substernal pain after eating that was relieved by belching. He had a history of hypertension and gout. The patient’s vital signs were normal.

The patient is a 47-year-old man who began to experiencefrequent headaches about 6 years before hepresented to a neurology clinic. The headaches rapidly progressedto become daily and almost constant. He describeda sensation of dull pressure in both temples that was presenton or within a few hours of awakening and that persistedfor the remainder of the day. He experienced a moreintense, disabling, throbbing pain in the same locationonce or twice a week, with photophobia and nausea, thatmight last 2 to 3 days. The patient took 2 to 6 over-thecounter(OTC) analgesic tablets each day-usually200 mg of ibuprofen. These would dull but not terminatethe pain.

A 67-year-old woman with insulin-dependent diabetesmellitus and uncontrolled hyperglycemia complained offatigue and malaise. For 2 years, a draining ulcer hadbeen present on the bottom of her left foot.

High-grade fever, chills, fatigue, malaise, and anorexia developed in a 35-year-old man following subclavian catheterization because of chronic renal failure of unknown cause. The patient, who had long-standing diabetes mellitus, was admitted to the ICU with the diagnosis of possible sepsis. The next day, he was found to have a grade 2/6 systolic murmur compatible with tricuspid regurgitation. This was confirmed when a 4-chamber echocardiogram (A) revealed a large single piece of vegetation (2 arrows) lying on the tricuspid valve, flapping in and out of the right ventricle. In a 2-dimensional echocardiogram of the right atrium and right ventricle (B), 3 arrows point to the vegetation. (RV, right ventricle; LV, left ventricle; RA, right atrium; LA, left atrium; TV, tricuspid valve.)

An 83-year-old woman is brought by her daughter for evaluation becauseof increasing confusion during the past few days. The patienthas early Alzheimer dementia, hypertension, and type 2 diabetes. She takes donepezil, 10 mg/d;lisinopril, 5 mg/d; and glipizide, 5 mg bid. She is unable to bathe and dress herself as well as previously,has been crying for no apparent reason, and has lost her appetite.

A 20-year-old woman presents with a 3-week history of a pruritic, progressivelyenlarging erythematous lesion on one arm. She has a cat and recentlystarted horseback riding lessons. She is otherwise healthy and takes nomedication.

Despite the manydouble-blind,placebo-controlledtrials thathave demonstratedthe efficacy of statins inreducing the risk of cardiovascularevents, a largenumber of patients who aretreated with these drugsstill experience suchevents. This may be becausepatients who requireintensive lipid lowering arenot receiving adequatedosages of statins.

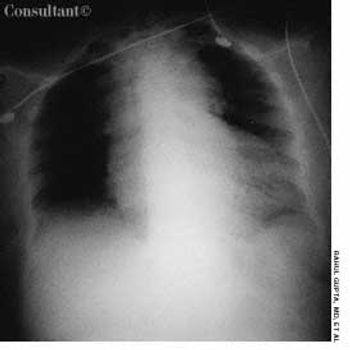
Two weeks earlier, this 66-year-old man had been hospitalized because of leftsided chest pain. However, cardiac evaluation revealed no abnormalities.

A 53-year-old man with type 2 diabetes mellitus and hypertension presented to the emergency department with pain in his left upper chest and back, neck, and shoulder. The pain increased with passive and active range of motion testing and decreased at rest. His physical examination was unremarkable except for restricted left shoulder movement and generalized tenderness in the left shoulder area.

A 30-year-old man presentedwith severe left flankpain radiating to his abdomenand gross hematuriaof 5 to 10 days’ duration.He also reported a 4- to 6-monthhistory of nausea with intermittentvomiting, anorexia, and progressiveweight loss. He took no medicationsand had no allergies.