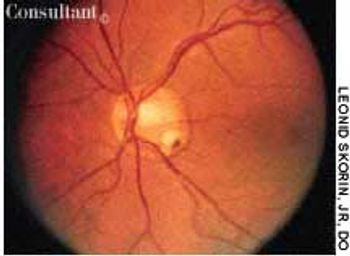
During a routine ophthalmologic examination, a round depression in the temporal region of the optic disc was found in a 35-year-old woman. Her past ocular history was noncontributory.

During a routine ophthalmologic examination, a round depression in the temporal region of the optic disc was found in a 35-year-old woman. Her past ocular history was noncontributory.

An 85-year-old white woman was brought to the emergency department (ED) with acute, severe left posterolateral chest wall pain of several hours' duration. The nonradiating pain was accompanied by shortness of breath. She denied palpitations, diaphoresis, syncope, or dizziness.

A 42-year-old woman sought medical advice for a facial rash of 4 weeks' duration. She denied any drug allergies, changes in her routine, or use of new laundry products.

A 61-year-old man with a history of squamous cell carcinoma was concerned about a tender nodule on his ear. He complained of exquisite tenderness with pressure, such as when lying on the affected side at night.
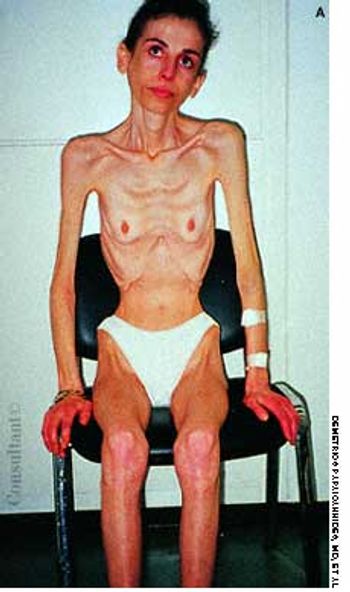
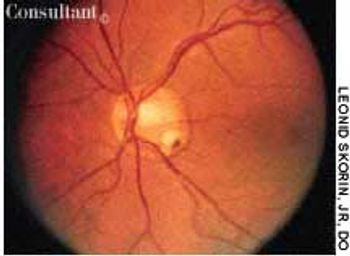
A 30-year-old woman was brought to the hospital with syncope, bradycardia, and hypotension. For the past 6 years, she had vomited after eating meals and after occasional episodes of binge eating.

Urinary incontinence is common--especially among older adults--but underdiagnosed. Many persons with this disorder are reluctant to discuss it with their physicians; often, only direct questioning can uncover the problem.

Advances in the understanding of multiple sclerosis (MS) have translated into aggressive treatment regimens that enhance patients' quality of life. In this article, we discuss the therapeutic options, especially treatments that are directed toward the underlying immunologic mechanisms of the disease. Because of its direct effect on quality of life, aggressive management of symptoms is emphasized.

Studies have indicated that depression occurs more frequently in adults with asthma than in the general population; however, few studies have investigated the relationship between depression and asthma outcomes. A recent study by Eisner and associates revealed noteworthy findings: depressive symptoms appear to be associated with poorer outcomes, including increased risk of hospitalization for asthma.

An 82-year-old woman complains that for the past 6 months, she has "not felt like herself." Previously, she was very active and energetic; in fact, 9 months earlier, she had vacationed in Hawaii. It now takes all of her energy just to get out of bed.

Confounding Factors in Treatment-Resistant Depression (Part 1): The Role of Subtyping and Bipolarity Michael I. Casher, MD, Daniel Gih, MD, Joshua D. Bess, MD, and Prachi Agarwala, MD

Combination therapy with pegylated interferon alfa-2a or alfa-2b and ribavirin (RBV) results in a greater rate of sustained virologic response (SVR) than that seen with standard interferon alone. Patients infected with hepatitis C virus genotype 1 require higher doses of RBV and a longer duration of therapy than do patients infected with genotype 2 or 3. Closely monitor patients for neuropsychiatric effects, especially depression, and hematologic and other toxicities. Because of the teratogenicity of RBV, strict birth control must be used throughout the course of treatment and for 6 months afterwards. Patients who have not demonstrated a 100-fold reduction in viral load after 12 weeks of therapy are unlikely to achieve SVR; discontinuation of therapy may be considered.

A 69-year-old man seen because of a pruritic pretibial rash of 3 months' duration. Started as reddish brown papules that slowly enlarged and changed.

The parents of a 16-year-old girl report that during the past several months, she has exhibited behavioral changes, irritability, increased anger, depression, and anxiety. The girl had previously been healthy, and there has been no recent illness or trauma.

Abstract: The laryngeal mask airway (LMA) and intubating LMA are valuable alternatives in patients in whom intubation has failed and who need oxygenation and ventilation immediately. The dual-lumen, dual-cuffed airway tube is effective in a variety of settings and can tolerate ventilation at pressures as high as 50 cm H2O; it is contraindicated in awake patients who have intact airway reflexes, caustic ingestions, and upper airway obstruction from a foreign body or pathology. Surgical airways are lifesaving techniques when intubation is unsuccessful or impossible through the mouth or nose. It may be particularly appropriate in patients with laryngeal or facial trauma, upper airway obstruction, or oropharyngeal injury. When patients aged 12 years and older cannot be ventilated by mask or intubated with traditional methods, surgical or needle cricothyrotomy is the procedure of choice. (J Respir Dis. 2005;26(7):298-302)

Multiple sclerosis, the most common cause of disability among young adults, can take years to diagnose because symptoms may wax and wane over time, and patients may not initially seek evaluation.

ABSTRACT: The management of chronic daily headache is difficult and complex. Those affected have a sensitive nervous system, and their predisposition for a low tolerance to sensory stimuli appears to be inherited. Under appropriate conditions, the equilibrium or balance between bombardment from painful stimuli and the regulatory systems that inhibit those stimuli is disrupted, allowing painful stimuli to become manifest at a greater intensity than in the nonmigraineur. Successful management depends on close adherence to nonpharmacologic approaches and pharmacologic regimens that desensitize the system and restore equilibrium. Comorbid conditions must be identified and treated as well.

A 37-year-old man presents with a large, pruritic, hyperpigmented, lichenified plaque on the left side of his upper back. A 7-year-old boy is brought for evaluation of a noninflammatory, nonscarring 3.5-cm area of alopecia in the right occipital region, which has been present for 6 months.

Over the past 5 to 10 years, there has been an increasing incidence of synthetic club drug use that has quietly permeated the adolescent and young adult culture. This review of MDMA, also known as Ecstasy, ketamine, GHB, and methamphetamine, provides a basic introduction to help practitioners get up to speed.

A 65-year-old woman with well-controlled hypertension comes in for a routine checkup. During the past 10 years, she has gained 25 lb and lost 1.5 inches in height.
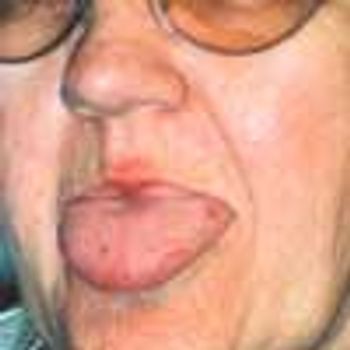
Lesions on the tongue and lips prompted a 61-year-old woman to seek medical attention. She also complained of craving ice and cold liquids. Her history included depression, which was treated with ser-traline, and lifelong recurrent epistaxis. She denied pulmonary or neurologic symptoms.

Primary care physicians are usually the first to see patients with joint pain; consequently they represent the "front line" of RA care. This fact-coupled with the projection that the number of rheumatologists is expected to decline by 20% during the next 2 to 3 decades-underscores the pivotal role that primary care clinicians are now expected to play in the early diagnosis of RA.

Abstract: For some patients with allergic rhinitis, symptoms can be reduced substantially by the use of allergen avoidance measures. However, many patients require pharmacotherapy, including antihistamines, decongestants, and intranasal corticosteroids, to adequately control their symptoms. The oral antihistamines are effective in reducing rhinorrhea, itching, and sneezing but are not effective against nasal congestion. Intranasal azelastine has been shown to be beneficial in patients with moderate to severe symptoms that are not sufficiently controlled by an oral antihistamine. Additional therapies include intranasal ipratropium, which specifically targets rhinorrhea, and cromolyn, which can reduce many of the symptoms of allergic rhinitis and can be used prophylactically. (J Respir Dis. 2005;26(4):150-162)

What steps can older patients take now to improve their health and quality of life and maintain their independence?

Cardiovascular disease is the chief cause of death among women. Nevertheless, in a recent survey of women, only 13% responded that their own greatest health threat was heart disease.

A 69-year-old woman was hospitalized with fever, chills, and nausea. Three weeks earlier, she had received a 2-week course of oral levofloxacin for pneumonia, which resolved. Her history included rheumatic heart disease; diabetes mellitus; depression; a hysterectomy; 2 mitral commissurotomies; nonrepairable mitral valve regurgitation, for which she received a St Jude Medical bileaflet valve; a left-sided cerebrovascular accident; and paroxysmal atrial fibrillation. Her medications included verapamil, furosemide, metoprolol, potassium chloride, metformin, nortriptyline, and warfarin. She denied tobacco and alcohol use.