
A 6-year-old girl (A) and an 11-year-old boy (B) each presentedfor evaluation of an erythematous, pruritic, papularrash that developed after swimming in a Wisconsin lake.Each child was otherwise completely healthy.

A 6-year-old girl (A) and an 11-year-old boy (B) each presentedfor evaluation of an erythematous, pruritic, papularrash that developed after swimming in a Wisconsin lake.Each child was otherwise completely healthy.

This 10-year-old boy presented forevaluation of a rash that developedduring a spring vacation on Florida’sAtlantic coast. After he had beenswimming in the ocean, a pruritic,erythematous, papular rash developedon his trunk, axillae, and groin. Approximately24 hours after the onsetof the rash, he experienced malaise,chills, and a sore throat. His past medicalhistory was unremarkable. Hehad been fully immunized and hadhad varicella infection.

A 43-year-old woman presented to the emergency department with a 4-day history of worsening erythema, swelling, and pruritus that developed on the face and progressed to the abdomen, back, and lower legs. In the past 2 to 3 days, fluid-filled blisters had arisen, followed by skin sloughing; the patient also reported subjective fevers. Another physician had prescribed naproxen for back pain 6 days earlier. The patient had a history of asthma, with rare inhaler use, and depression, for which she had taken citalopram for 2 years.

A 72-year-old woman presented for evaluation of a large swelling onher dorsal wrist, which had been present for 2 years. The protuberancewas not painful or tender; the patient was otherwise in goodhealth.

For 3 days, a 47-year-old woman had a painful red swelling on her finger.The patient--a cellist--had tried to lance the lesion at home, but itprogressively worsened and was now “throbbing.” She denied fever andnail biting.

Swelling of the lower legs broughtthis 57-year-old woman to a familypractice clinic. She had a history ofhyperthyroidism with weight loss,tachycardia, and anxiety. This conditionwas confirmed with blood testsand radioactive iodine uptake testing.

A mildly painful, nonpruritic rash on the forearms and legs prompted a 42-year-old man to go to the emergency department. The patient noted the rashwhen he awoke that morning. He had had joint pain and fever for the past7 days and generalized malaise with chills that began about 3 days earlier.He had no significant medical history.

Hyperpigmentation is seen on the cheeks and eyelids of a 36-year-old woman.She became hyperthyroid at age 19 years, with accompanying exophthalmosand hyperpigmentation, following the birth of her first child. Thyroidectomywas carried out at that time, and the patient has been receiving thyroid replacementtherapy ever since. The hyperpigmentation, an uncommon accompanimentof hyperthyroidism, has persisted.

ABSTRACT: Acute scrotal pain, a high-riding testicle, and the absence of the cremasteric reflex on the affected side signal testicular torsion-a surgical emergency. The pain associated with torsion of the appendix testis is usually of gradual onset and is exacerbated by movement. The tenderness is often localized over the infarcted appendix, and the infarction may be visible through the scrotal skin (the "blue dot sign"). Pain associated with epididymitis is usually gradual in onset; the patient may complain of dysuria, increased frequency, and discharge, particularly if the causative pathogen is Chlamydia trachomatis or Neisseria gonorrhoeae. Hydroceles are smooth and nontender, and the scrotum transilluminates. If the scrotum does not transilluminate and compression of the fluid-filled mass toward the external ring completely reduces the mass, then a hernia is the more likely diagnosis. A patient with a varicocele typically complains of a sensation of heaviness and of "carrying a bag of worms."

A painful rash suddenly developed on the chest wall of an otherwise healthy 8-year-old girl. Examination of the rash revealed grouped vesicles with an erythematous base in a linear distribution along the T5 dermatome. The child had not been vaccinated with varicella vaccine and had had chickenpox 3 years earlier.

For more than 20 years, a 55-year-old man had a faintly erythematous, papulosquamousrash with arciform borders on his groin and waistline. The rashhad been treated with a variety of medications. Topical and oral antifungalsand antibiotics and topical corticosteroids had been used but to no avail. Nolaboratory tests had been performed.

For 1 year, a 30-year-old man had an intermittent rash that was confined to thearea of his jockey shorts; no other part of the body was affected. The patientreported that the pruritic eruption arose and disappeared spontaneously andwas more prominent during the heat of summer.

A 50-year-old man had a long-standing rash on both soles. The patient’s toenails were yellow and dystrophic. These physical findings strongly suggested moccasin-variety tinea pedis and onychomycosis.

For years, a 39-year-old man had an eruption on his hand, which seemed to becontrolled with topical corticosteroids. The patient was a rancher.
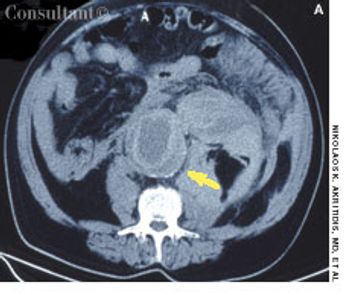
Severe abdominal pain radiating to the back prompted a 72-year-old man to go to the emergency department (ED). The patient had experienced similar pain 2 days earlier and was treated at another hospital for renal colic on the basis of concomitant microscopic hematuria. He had a history of poorly controlled hypertension.

For 2 months, an asymptomatic rash had been present on the upper arms of a 16-year-old boy of normal weight. The rash, as seen on the patient’s right arm, consisted of abundant fine papules. He had no other lesions.

7-year-old boy presented with an asymptomatic cystic lesion on the lateral aspect of the left ankle of 4 months’ duration. There was no history of trauma. The mass fluctuated in size; it was smaller when the child was recumbent and larger when the child was upright.

A 33-year-old active-duty soldier who had been in Iraq for 6 months presented with a depressed lesion on his left lateral elbow of several months’ duration. It was neither healing nor enlarging. (The yellowish tint to the skin in the photograph was from a topical iodine solution.)

A painless swelling on the dorsum of the scalp had been present for many years in a 36-year-old man. An increase in the size of the lesion prompted the man to seek medical evaluation.

The continuous use of a corticosteroid cream briefly relieved the pruritus of anannular, papulosquamous eruption on the left anterior thigh of a 50-year-oldwoman. The lesion was present for 6 months and grew larger with applicationof the topical corticosteroid.

For several months, a 49-year-old woman has had asymptomatic loss of pigmenton her shins. She has no history of injury to the area.What is your clinical impression?
During a routine physical examination, a white forelock was noted on a 54-year-old man. The patient stated that the discolored patch of hair had been present since adolescence. Other than mild hearing loss, he had no significant personal or family medical history.

A 46-year-old man with diabetes presented for evaluation of gradual fingernail deterioration, which had failed to respond to several courses of griseofulvin and a recent 3-month course of daily terbinafine. The patient-who worked as a bartender-was otherwise healthy.

For several weeks, a 78-year-old woman had an intensely pruritic, diffuse, raised, slightly scaly, erythematous rash that persisted despite the use of several over-the-counter topical medications (such as hydrocortisone and clotrimazole cream). Since her last visit about 3 months earlier for a blood pressure reading, she had been well except for 2 episodes of night sweats.

The American Cancer Society predicts that 55,100 cases of melanoma will be diagnosed in 2004.1 More than 1 million new cases of basal cell and squamous cell carcinoma are expected.2