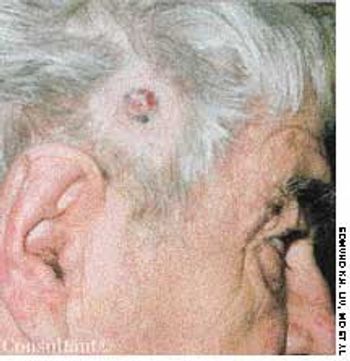
A 67-year-old man had been aware of a painless, firm, red nodule that had been growing slowly on the right temporal area for 1 year. The lesion occasionally bled.

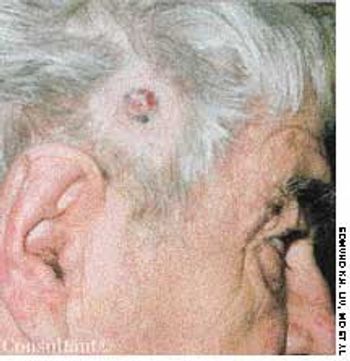
A 67-year-old man had been aware of a painless, firm, red nodule that had been growing slowly on the right temporal area for 1 year. The lesion occasionally bled.

A 76-year-old woman had a 40-year history of rheumatoid arthritis (RA). She had repeatedly refused treatment with disease-modifying drugs, including methotrexate. Nodules began to develop 15 years after the initial diagnosis; they recurred after surgical removal.

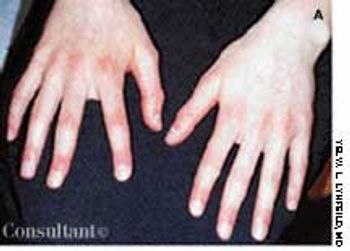
A 65-year-old woman, who was confined to a wheelchair because of severe rheumatoid arthritis, was concerned about nodules that had erupted on her fingers and hands during the previous 3 weeks. Her medical history included colon cancer, chronic renal insufficiency, anemia, and hypertension. The nonpruritic nodules were painful when they began to form under the skin; however, once they erupted, the pain disappeared.

A variety of rheumatic diseases-systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), and the vasculitides among them-manifest as “lumps, bumps, and holes” involving the extremities. Each of these diseases works through specific mechanisms on different structures of the skin to produce a distinctive pathology. In doing so, each provides clues to the cause, which the history and physical examination can help confirm.

This 64-year-old woman has had rheumatoid arthritis for 15 years; her hands show classic rheumatic changes. She also had a leg ulcer that had failed to heal in 8 years despite three skin grafts.

Various types of cutaneous lesions may occur in association with RA, including rheumatoid nodules, rheumatoid neutrophilic dermatitis, vasculitis, palpable purpura, and pyoderma gangrenosum. Many of these manifestations-including rheumatoid nodules-are specific for RA. The presence of these nodules is associated with seropositive disease and with a more severe, erosive clinical presentation. The nodules appear in 20% to 30% of patients with RA. Sites of predilection are those subject to shear stress, including the subcutaneous tissues over the extensor aspects of the elbow region, over the sacrum in bedridden persons, and at the pericardial and pleural surfaces.

Cutaneous and subcutaneous lesions of the extremities may be clues to the presence of rheumatic diseases such as systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), and the vasculitides. The history and physical examination can generally help confirm the cause. Skin biopsy is sometimes necessary for a definitive diagnosis; useful results depend on a technique that gives the depth necessary to see the pathology and proper interpretation of biopsy specimens by an experienced dermatopathologist.

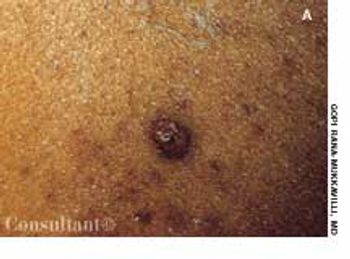
Pyoderma gangrenosum (PG) is a chronic, recurrent condition characterized by cutaneous ulceration. In half of patients, PG is associated with an underlying illness, such as inflammatory bowel disease, RA, SLE, or a lymphoproliferative disorder.

This 20-month-old girl was born to a 28-year-old mother at 38 weeks' gestation. The pregnancy was uncomplicated, and vaginal delivery was normal. The infant sat with support at 10 months of age, sat without support at 12 months, crawled at 13 months, and walked at 18 months. She had not yet begun to talk at 20 months. The child was noted to have frequent laughing episodes and often made flapping movements with her hands.

A 29-year-old man presented with a complaint of venereal warts and a long history of mild psoriasis, which he had treated with fluocinolone. He returned 3 months later complaining of chest congestion of 10 days' duration; it had been treated with ciprofloxacin at an urgent care facility.

Loss of pigmentation is noted around the left eye of a 49-year-old African-American man-the same eye in which he has a detached retina. In addition, the patient's hearing is impaired on that side.

A 68-year-old man presented to the emergency department (ED) complaining of an itchy rash over his body. His past medical history included hypertension, contact dermatitis, and penicillin allergy.

Highly pruritic, 2- to 4-mm, papular lesions with central ulceration erupted on the back of a 66-year-old woman. She had had 2 similar outbreaks in the past. The patient was taking conjugated estrogens, alprazolam, and alendronate.

A 43-year-old woman requested removal of a lesion from her left axilla because it had recently become irritated. The polypoid lesion with dried terminal ulceration had been present for 17 years.

Although alopecia areata is an inflammatory, autoimmune type of hair loss, it is characterized as a nonscarring type; the hair grows back in all but extremely long-standing cases.

The left ear of a 1-month-old infant girl shows a congenital papillomatous lesion at the preauricular area. She had no other apparent abnormalities.

While doing yard work, a man experienced acute, severe, burning pain on relatively brief contact with the caterpillar Megalopyge opercularis. The lesion shown in the photograph developed subsequently. Each red papule represents the site of direct cutaneous envenomation by the insect's poisonous body hairs. The caterpillar can vary in color from white to dark brown, depending on the surroundings and time of year. The fuzzy hairs resemble a cat’s fur; hence the nickname “puss.”

The patient reported that he had noticed the facial eruption a couple of months earlier. On examination, the lesion appeared more plaque-like and dense than is typical of rosacea. The differential diagnosis included lupus, mycosis fungoides, rosacea, and angiosarcoma.

The lesions seen here developed shortly after a 54-year-old woman started psoralen plus UVA (PUVA) therapy for psoriasis. This is acne estivalis, an uncommon actinic, acneiform eruption. The firm, red, monomorphic papules are most commonly found on the shoulders, arms, neck, and chest. Histologically, they resemble steroid acne. Lesions develop in the spring, peak in the summer, and resolve in the fall without scarring.

Seen here are a 38-year-old Native American woman and her 20-year-old daughter, each of whom has had a relapsing eruption for several years. Pruritic, red to red-brown plaques develop on their faces and necks and on the dorsal surface of their hands. Scattered brown and hypopigmented macules as well as some scaling and slight erythema appear on their lower lips. The women stated that the eruptions flare each spring and gradually improve throughout the rest of the year. The daughter's lesions were more acute at this time and had developed during the preceding 3 days.

The frontal and bitemporal hair recession generally seen in men with androgenetic alopecia is not typical in women, who instead tend to undergo a diffuse thinning of hair on the crown.
Cyanosis involving the hands and toes of a 12-year-old girl was first noted 3 months before medical evaluation was sought. Her fingers and palms were red, the nail beds were cyanotic, and her palms were cold and sweaty. The girl's toes were cyanotic when she was standing. Her hands and feet reverted to a normal color when the limbs were elevated.

The rash of tick tularemia is seen here on the arm of a 5-year-old boy. He also had a tick bite on his back that became necrotic and ulcerated. Within 2 weeks of his having been bitten, axillary lymph nodes developed.
A 37-year-old man presented with fever, chills, myalgia, headache, and left-sided pleurisy of 2 weeks' duration. He also complained of weight loss and loss of appetite. The patient had recently returned from a family visit to Missouri.

The wounds on the back of this boy's head resulted from an encounter with his neighbor's dog. The youngster's anxious parents brought him in for evaluation 1 hour after he was bitten.